Pterygium is a benign, fibrovascular overgrowth of bulbar conjunctiva extending onto the cornea and has been associated with ultraviolet (UV) light exposure. The prevalence of pterygium worldwide varies between geographical zones but has been reported to range between three and 30% [1].
In some advanced cases the pterygium obstructs the visual axis, and this is considered an absolute indication for surgical intervention. Additionally, this condition can also affect the corneal surface causing irregularities and inducing astigmatism and surface asymmetry. This can prompt surgical intervention earlier in the course of the disease [2]. Other indications for surgical intervention include restriction in eye movements, chronic redness, foreign body sensation and cosmetic reasons [1].
Pterygium is thought to result of common ocular surface lesions that originate from limbal stem cells altered by chronic UV exposure [3]. Histopathological changes include squamous and goblet cell hyperplasia. Changes and deficiency of limbal epithelial stems cells, normally maintaining the corneal transparency and homeostasis, may lead to the development of conjunctival epithelium infringement onto the corneal surface. The condition usually appears at the nasal limbus where UV irradiation is 20-fold stronger and invades centripetally the cornea and its prevalence is high in the “pterygium belt” between 30 degrees north and 30 degrees south of the equator [1].
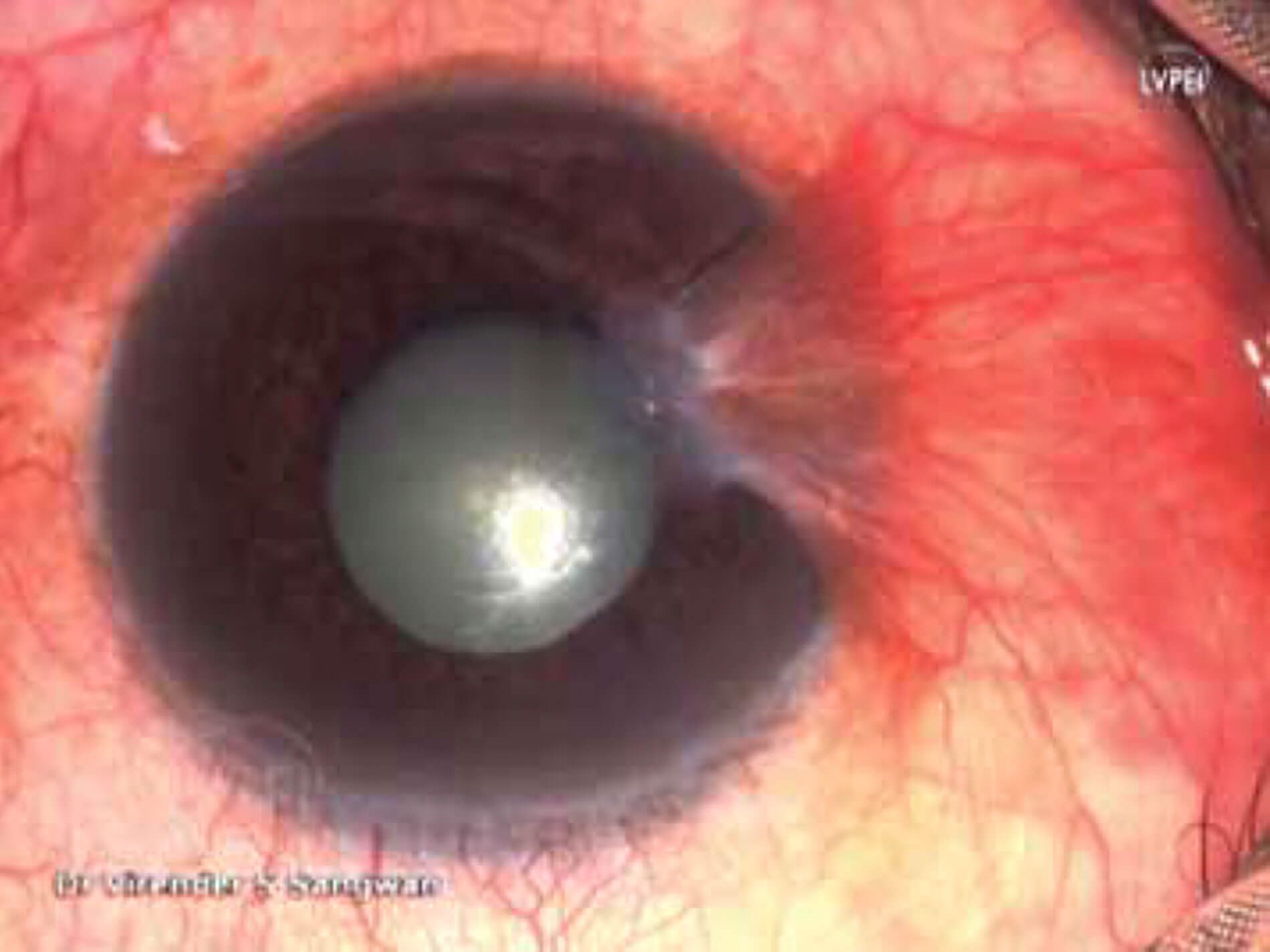
Figure 1: Grade III pterygium: parts of the eye are painted
with betadine and draped maintaining sterility.
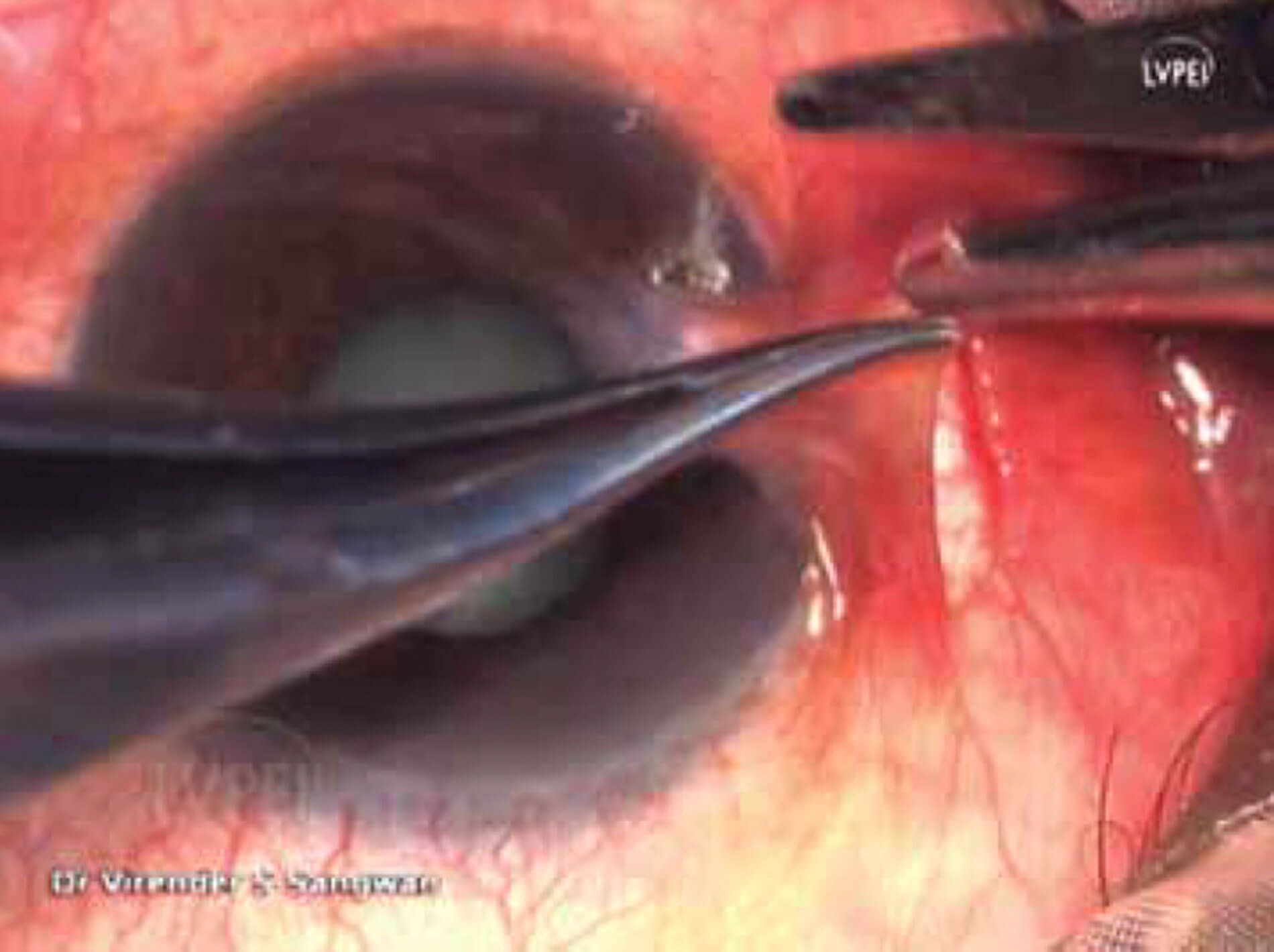
Figure 2: Using a Lim’s forceps, the body of pterygium is grasped, and subconjunctival
dissection done with Vannas scissors from forniceal approach.
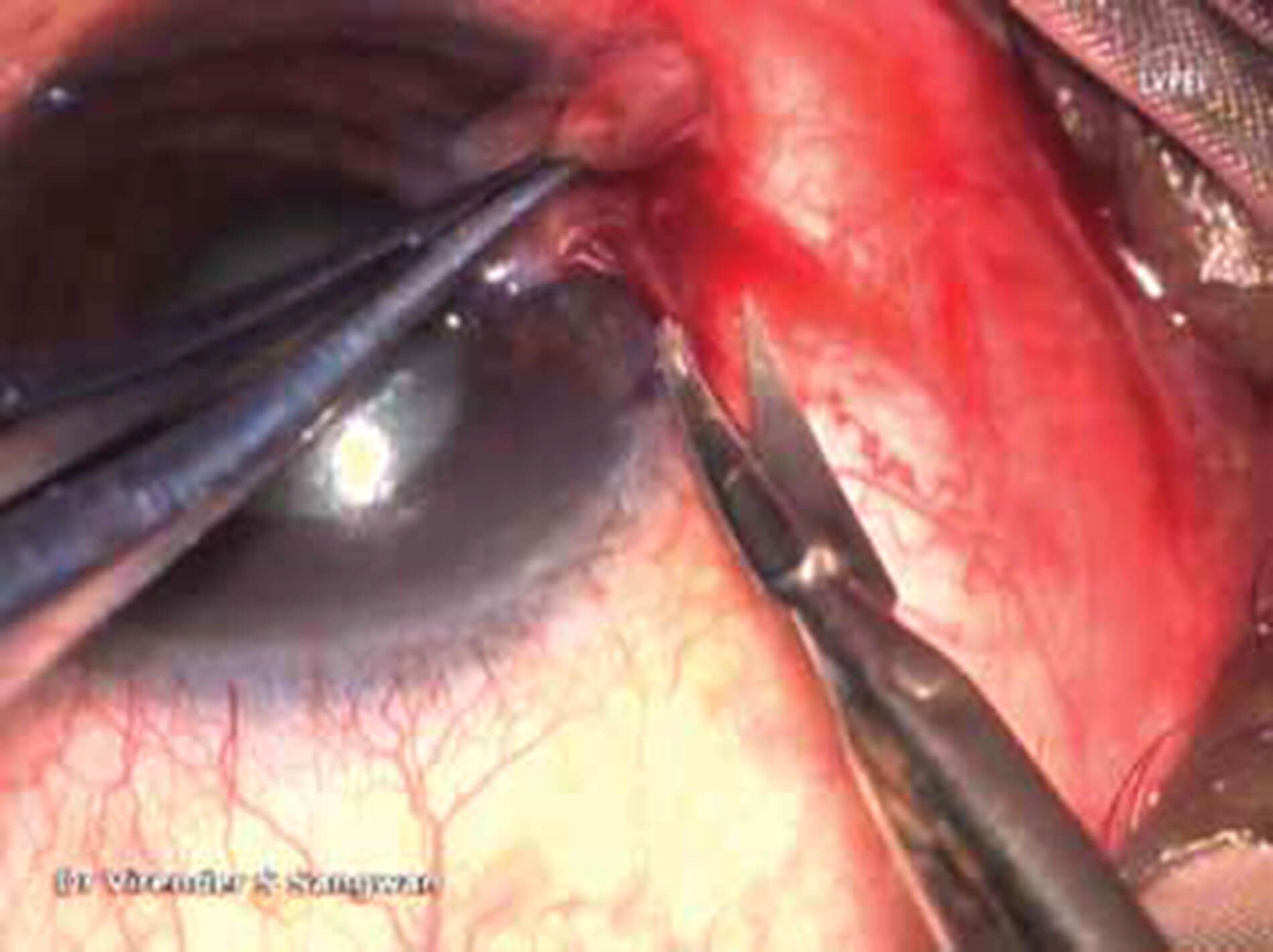
Figure 3: Once the plane is identified, the head of the pterygium
is separated and peeled off using forceps and Vannas scissors.
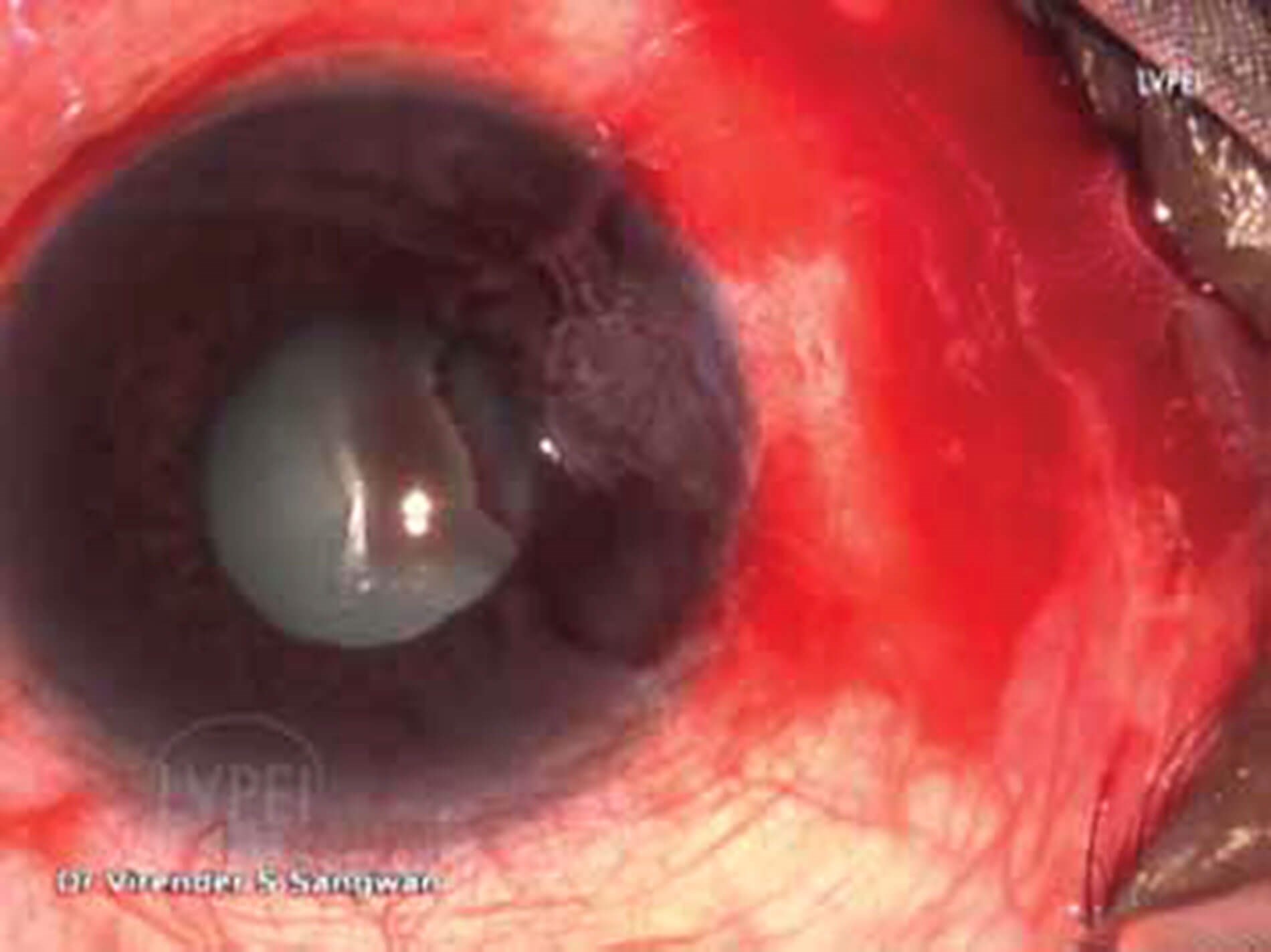
Figure 4: After the pterygium is separated and peeled off,
the conjunctiva falls back toward the fornix.
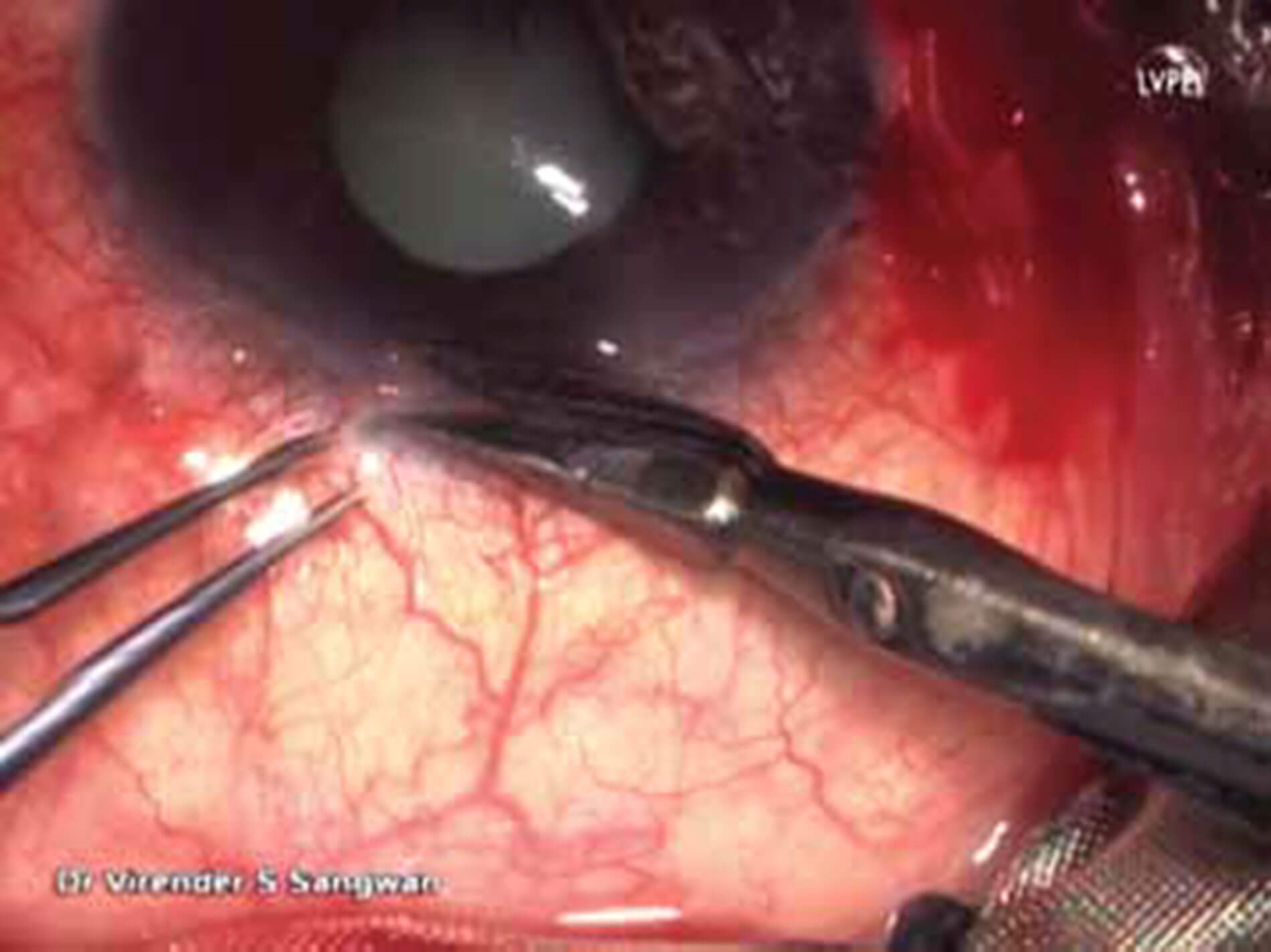
Figure 5: Landmark for snip biopsy for stem cells to be taken near the limbus.
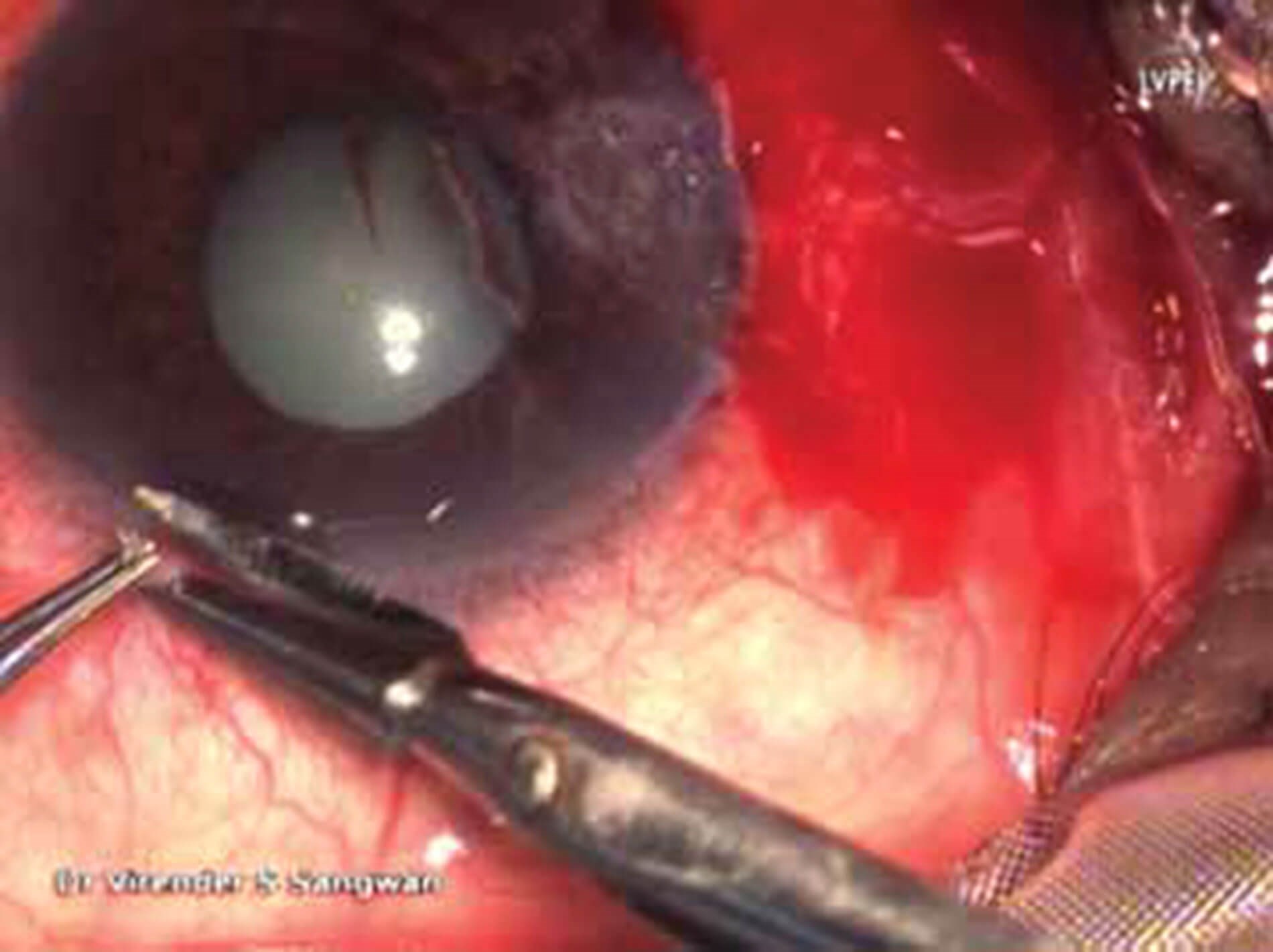
Figure 6: Snip biopsy of the limbus with stem cells is
taken using Lim’s forceps and cut with Vannas.
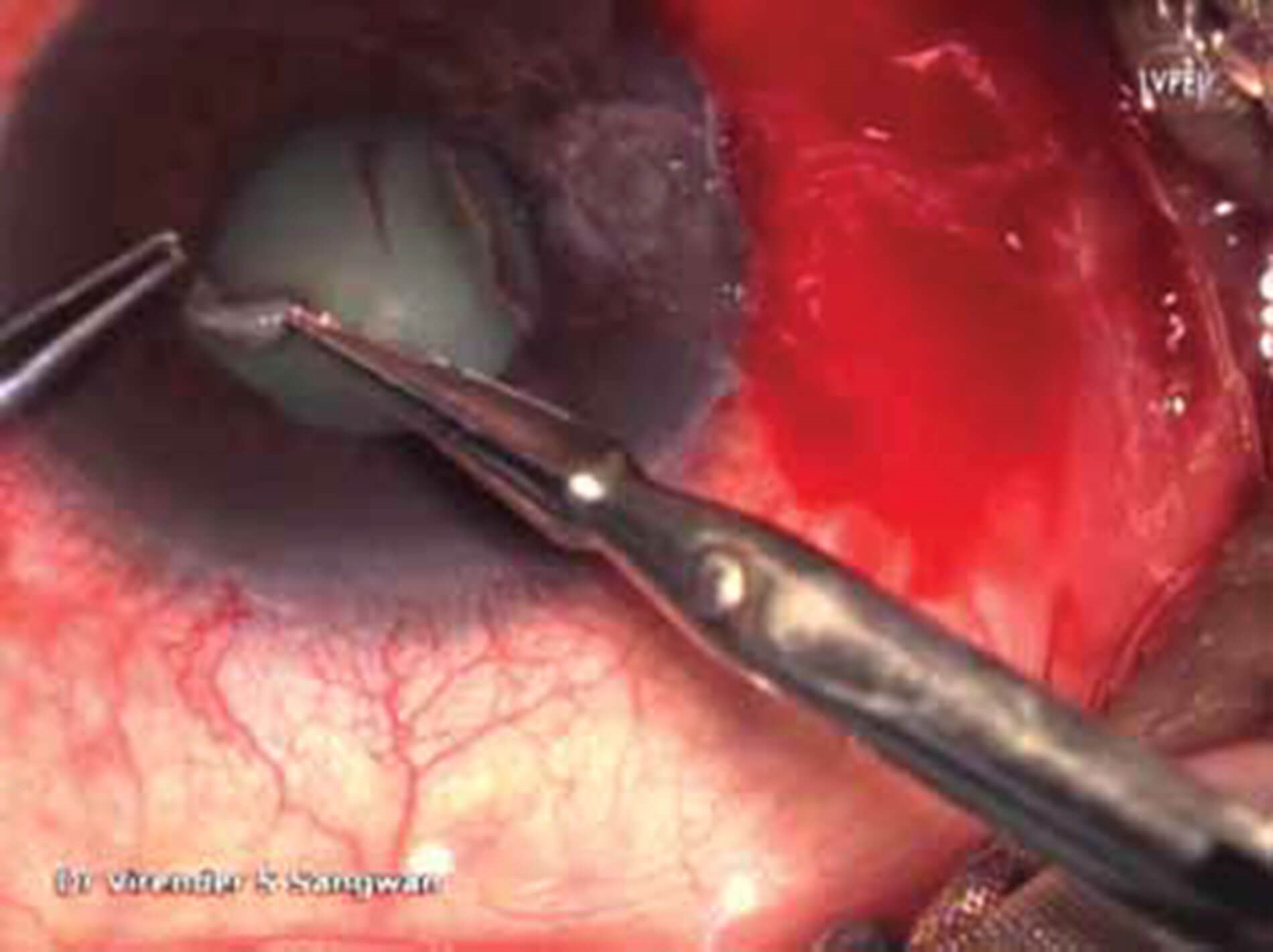
Figure 7: Snip biopsy of the limbus with stem cells is
chopped into three to four pieces using Vannas.
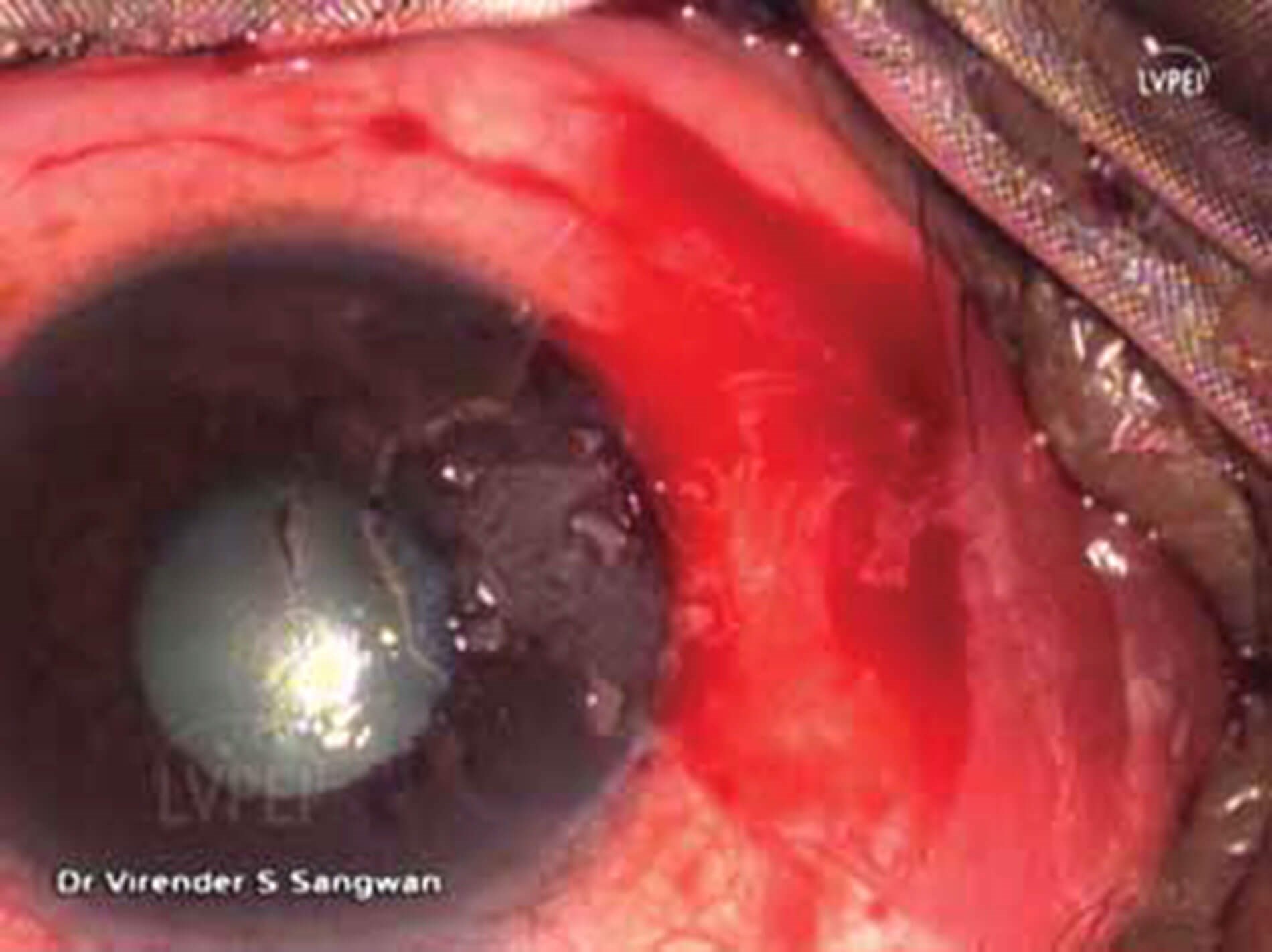
Figure 8: Pieces are placed over the limbus and the bare
sclera and secured using fibrin and thrombin glue.
Pterygium is often corrected with excision. The first technique introduced was simple excision with bare sclera but recurrence rates after surgery varied from 24% to 89% [4]. Several techniques have been developed to try to reduce such recurrence rates. Applications of cytotoxic agents such as mitomycin C have been tried. However, complications such as inflammatory scleritis and scleromalacia have been reported in some cases. Amniotic membrane transplantation has also been proposed. The advantages of using this technique include inhibition of angiogenesis and the covering of a large area without the need to harvest health conjunctiva [5]. The usage of conjunctival autograft that uses superotemporal bulbar conjunctiva and involves suturing the graft over the exposed scleral bed after excision of the pterygium has been reported to be associated with a two to 12% recurrence rate and to be associated with lower complication rates [1]. Additionally, the cosmetic results are usually better with conjunctival autograft when compared to amniotic membrane transplantation [5]. However, conjunctival-limbal autograft cannot be performed in cases where a large defect needs to be covered or in patients where the conjunctiva needs to be preserved for future glaucoma surgery to avoid conjunctival scarring at the harvesting site [6]. Other techniques include radiation, photodynamic therapy, and antiangiogenic agents that have been introduced over the years to try to overcome recurrence.
“Considering the physiopathology of pterygium, newer techniques combine the use of sclera covering with graft with a small autologous simple limbal epithelial transplant (mini-SLET) to provide stem cells at the limbal area”
Stem cells are poorly differentiated cells with a high self-renewal capacity with an increased potential for error-free proliferation and cell division [5]. These cells have the capacity of producing a large number of differentiated, functional progeny and of regenerating the tissue after injury. In the corneal epithelium, the stem cells are located in the basal layer at the limbus [7]. This population of limbal epithelial stem cells (LESC) are responsible for maintaining the epithelium throughout life by providing a constant supply of daughter cells that replenish those constantly lost from the ocular surface during normal wear and tear and following injury. LESC deficiency leads to corneal opacification, inflammation, vascularisation and discomfort [8].
Considering the physiopathology of pterygium, newer techniques combine the use of sclera covering with graft with a small autologous simple limbal epithelial transplant (mini-SLET) to provide stem cells at the limbal area. In practical terms, this can be achieved by placing pieces of limbal epithelium in the affected limbal area covered by a second graft using fibrin glue with good results in avoidance on recurrence [9]. Loomba et al. described the steps of the surgical technique. After careful draping in a sterile manner, forceps are used to grasp and dissect the subconjunctiva. Once the plane is identified, the head of the pterygium is separated and peeled off. A snip biopsy of the limbus with stem cells is taken and chopped into three to four pieces, that are placed over the limbus and the bare sclera and secured using fibrin and thrombin glue. After, a bandage contact lens is placed over the cornea and the eye is patched after applying betadine eye drops. The patch is removed the next day and topical steroids and antibiotics are used for the postoperative period [5].
Outcomes of this technique have been reported in the literature. A case series of nine patients showed that at eight months follow-up, the limbal epithelial pieces were no longer visible, the area of the limbal biopsy showed no focal stem cell deficiency and the cosmetic results were favourable, and we had no cases of recurrence [6]. A review from Sangwan et al. reported that SLET offers a cheaper and perhaps safer alternative compared to others and that clinical results were comparable to other stem cell techniques described in other papers, but this was when treating limbal stem cell deficiency in general [10]. In another case series of four cases of recurrent pterygium the SLET procedure went without complication and with good outcomes [11]. Interestingly, a randomised controlled trial compared outcomes between mini-SLET and conjunctival autograft (CAG) fixation with fibrin glue after excision of pterygium. Ninety-two eyes with primary nasal pterygium were prospectively randomised into a CAG control arm and a mini-SLET study arm. The mini-SLET cohort showed less recurrence rate with reduced postoperative symptoms and other complications [12]. Another study also compared CAG and mini-SLET for primary pterygium excision in 2022 in 264 eyes and reported that overall recurrence rate was very low and comparable between mini-SLET and the established technique of CAG after performing the primary pterygium excision in groups that were comparable at baseline. They reported longer surgical time being needed for mini-SLET (20.33 ±1.28 min versus 12.01 ±1.26 min) but concluded that this novel technique appears to be a viable option for the management of primary pterygium [13]. Other studies have also reported the conjunctival autograft surgery with stem cells technique to be safe, effective, and useful preventing recurrence [9,14].
The results and outcomes so far appear to be promising. Further research should focus on the evaluation of clinical success against other more established techniques through high quality research studies.
Take Home Messages
-
Pterygium is a benign, fibrovascular overgrowth of bulbar conjunctiva extending onto the cornea and has been associated with ultraviolet light exposure and other modifiable risk factors.
-
Pterygium can obstruct the visual axis and modify the corneal surface inducing astigmatism.
-
Limbal epithelial stem cells are responsible for maintaining the epithelium throughout life by providing a constant supply of daughter cells.
-
The novel technique of small autologous simple limbal epithelial transplant has shown promising results in the surgical treatment of pterygium.
References
1. Singh SK. Pterygium: epidemiology prevention and treatment. Community Eye Health 2017;30(99):S5.
2. Shahraki T, Arabi A, Feizi S. Pterygium: an update on pathophysiology, clinical features, and management. Therapeutic Advances in Ophthalmology 2021. Epub ahead of print.
3. Chui J, Coroneo MT, Tat LT, et al. Ophthalmic pterygium: a stem cell disorder with premalignant features. American J Pathol 2011;178(2):817-27.
4. Jaros PA, DeLuise VP. Pingueculae and pterygia. Surv Ophthalmol 1988;33(1):41-9.
5. Loomba A, Sangwan VS. Stem Cell Applications in Pterygium. In: The Art of Pterygium Surgery: Mastering Techniques and Optimizing Results. New York, USA; Thieme; 2020:94.
6. Eirck HB, Amescua G, Navas A, et al. Minor ipsilateral simple limbal epithelial transplantation (mini-SLET) for pterygium treatment. Br J Ophthalmol 2015;99(12):1598-1600.
7. Dua HS, Azuara-Blanco A. Limbal stem cells of the corneal epithelium. Surv Ophthalmol 2000;44(5):415-25.
8. Notara M, Alatza A, Gilfillan J. In sickness and in health: corneal epithelial stem cell biology, pathology and therapy. Exp Eye Res 2010;90(2):188-95.
9. Mahdy MAES, Bhatia J. Treatment of primary pterygium: role of limbal stem cells and conjunctival autograft transplantation. Eur J Ophthalmol 2009;19(5):729-32.
10. Sangwan VS, John AH. Simple limbal epithelial transplantation. Curr Opin Ophthalmol 2017;28(4):382-86.
11. Mednick Z, Boutin T, Einan-Lifshitz A, et al. Simple limbal epithelial transplantation for recurrent pterygium: A case series. Am J Ophthalmol Case Rep 2018. Epub ahead of print.
12. Sati A, Banerjee S, Kumar P. Mini-simple limbal epithelial transplantation versus conjunctival autograft fixation with fibrin glue after pterygium excision: a randomized controlled trial. Cornea 2019;38(11):1345-50.
13. Jha A, Abhay S. Conjunctival autograft versus combined amniotic membrane and mini-simple limbal epithelial transplant for primary pterygium excision. J Ophthalmic Vis Res 2022;17(1):4-11.
14. Abdalla, WM. Efficacy of limbal-conjunctival autograft surgery with stem cells in pterygium treatment. Middle East Afr J Ophthalmol 2009;16(4):260.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME






