 *First author
*First author
Students have very little exposure to ophthalmology during their years at medical school. Teaching consists of a handful of lectures followed by a short placement in which students are expected to practise histories and examinations on patients with little to no understanding of which questions to ask and what signs to look for.
This guide aims to fill that gap by giving medical students a systematic approach to the ophthalmology patient. This guide aims to consolidate knowledge so that students may approach patients with eye complaints with confidence whether that be in examinations, on the ward or in a primary care/Emergency department setting.
History
The history is the most important part in assessing a patient with eye symptoms. The main red flag symptoms which may indicate the presence of sight threatening condition include:
- Sudden vision loss
- Pain particularly on eye movement
- Redness
- Photophobia
- Double vision (diplopia)
- Flashing lights or floaters
- Associated headache / fever
- Foreign body / chemical injury / trauma to the eye
- Temporal tenderness or jaw claudication
Other symptoms to investigate would include watering, itching, discharge (clear or purulent, stickiness in the eye particularly on waking). It is important to decipher general features including, duration, onset, triggers, which eye was affected or both.
Considering the patients past medical history is also vital as many ophthalmic presentations can be associated with a number of systemic diseases particularly auto immune conditions.
Asking about contact lens use is also important as these patients are more at risk of developing corneal infections or ulcers. Past ocular history includes recent procedures, previous eye surgeries, laser or any other known conditions.
Finally, a comprehensive drug history may help to point towards the diagnoses particularly the use of eye drops. It is also important to remember that some drugs can precipitate conditions such as acute angle closure glaucoma in at-risk patients. These drugs include salbutamol, selective serotonin reuptake inhibitors (SSRIs), anticholinergics and antihistamines.
Examination
A thorough examination of a patient presenting with eye symptoms would include taking a set of observations and general examination by the patient bedside to ensure the patient is stable and to determine the presence of any systemic features. It is also important to remember to check both eyes even if patients are only presenting with symptoms in one eye – this is often missed by many clinicians!
General Examination
A closer examination of the face is important to assess for any local skin reactions, rashes, lymphadenopathy and assessing the external eye to check for any obvious pathology of the eye lids or surrounding area.
Lids
- Assess the position – is there any ptosis? Redness or swelling which may suggest periorbital cellulitis?
- Assess for the presence of any lumps or bumps such as chalazion or styes.
- Check the lashes for any blepharitis.

Figure 1: A chalazion [1].
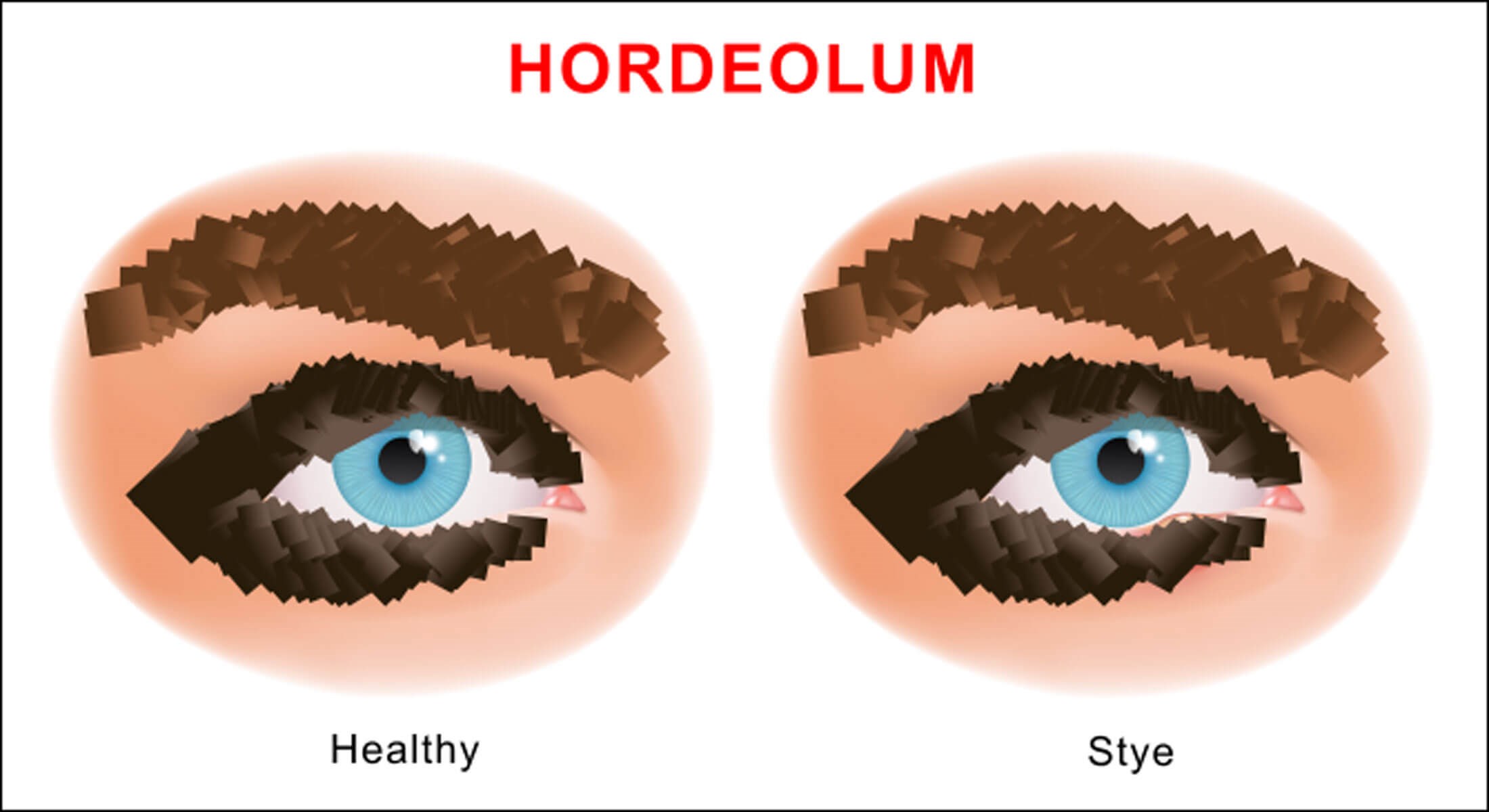
Figure 2: A stye [2].
Vision
- Visual acuity must be measured and checked with the patient’s usual glasses / contact lens.
- This can be done formally with a Snellen chart or if not available can be grossly assessed with reading material.
- Visual fields to assess for any field losses.
- Colour vision using Ichihara plates.
Pupils
- Size.
- Shape – abnormal shapes could be due to previous surgeries or changes to the iris.
- Reflexes such as reaction to light, accommodation, red reflex.
- Relative afferent pupillary defect – present in retinal or optic nerve disease. A light shone in the healthy eye causes equal constriction of both pupils, when rapidly shone in the eye with a lesion in the afferent pathway there is dilatation of both pupils.
- Presence of clinical sign – ciliary flush, irregular iris shape (present in anterior uveitis), hazy cornea (may suggest acute angle closure glaucoma).
Conjunctiva
- Assess the colour – presence of redness may suggest pathology such as acute angle closure glaucoma, keratitis, uveitis or conjunctivitis. Pallor (as seen in anaemia), blebs (due to cysts), ulcerations.
- Look for foreign bodies asking patients to look far left and far right.
- Note any discharge which may be purulent (bacterial conjunctivitis) or watery (foreign body or viral conjunctivitis), presence of follicles or papillae (little bumps on the conjunctival surface).
- Lid eversion may be necessary particularly if trying to find a foreign body.
Cornea
- Assess for clarity, opacification – hazy cornea is a sign seen in acute angle closure glaucoma.
- Fluroscein staining can be used to look for epithelial defects such as abrasions or ulcers.
- Dendritic ulcers which appear as tree branch-shaped lesions are suggestive of herpetic disease and need urgent ophthalmic review.
- Any suspicion of penetrating injury needs referral to a senior ophthalmologist.

Figure 3: A hazy cornea as seen in acute angle closure glaucoma [3].
Anterior chamber view is limited without a slit-lamp but can still be assessed to look for obvious signs such as:
- Hypopyon – fluid level of pus as seen in anterior uveitis.
- Hyphaema – blood collection seen in eye trauma.
It is also important to measure intra-ocular pressure to check for acute angle closure glaucoma although instruments to measure this are not always available.

Figure 4: Hypopyon [4].
Ophthalmoscopy
This is rarely done as doctors are not regularly trained or up to date in their skills however it is good practice to examine the fundus for completeness. If necessary, dilating drops can be used for a clearer view such as tropicamide or phenylephrine if you are trained in administering them. It is important to warn the patient they will not be able to drive for some hours after using the drops and always check the RAPD before giving mydriatic drops.
First explain to the patient: “I am going to examine the back of your eyes by shining a light into your eye and coming very close to your face”. Stand on the side you with to examine and always examine both eyes.
Elicit the red reflex then follow this towards the eye to look for the optic disc. Once in focus assess for the following:
- Colour of the fundus e.g., pallor sugging optic atrophy or red blotchy haemorrhages suggesting retinal vein occlusion.
- Look for features of papilloedema blurred optic disc margins, engorged veins.
- Assess vascular branches looking for aneurysms or exudates (diabetic retinopathy).
- Assess the macula looking for drusen, cherry red spots or haemorrhages suggesting ARMD.
- Retinal detachment and retinal haemorrhages may sometimes be seen by experienced practitioners however ideally slip lamp examination would visualise this better.
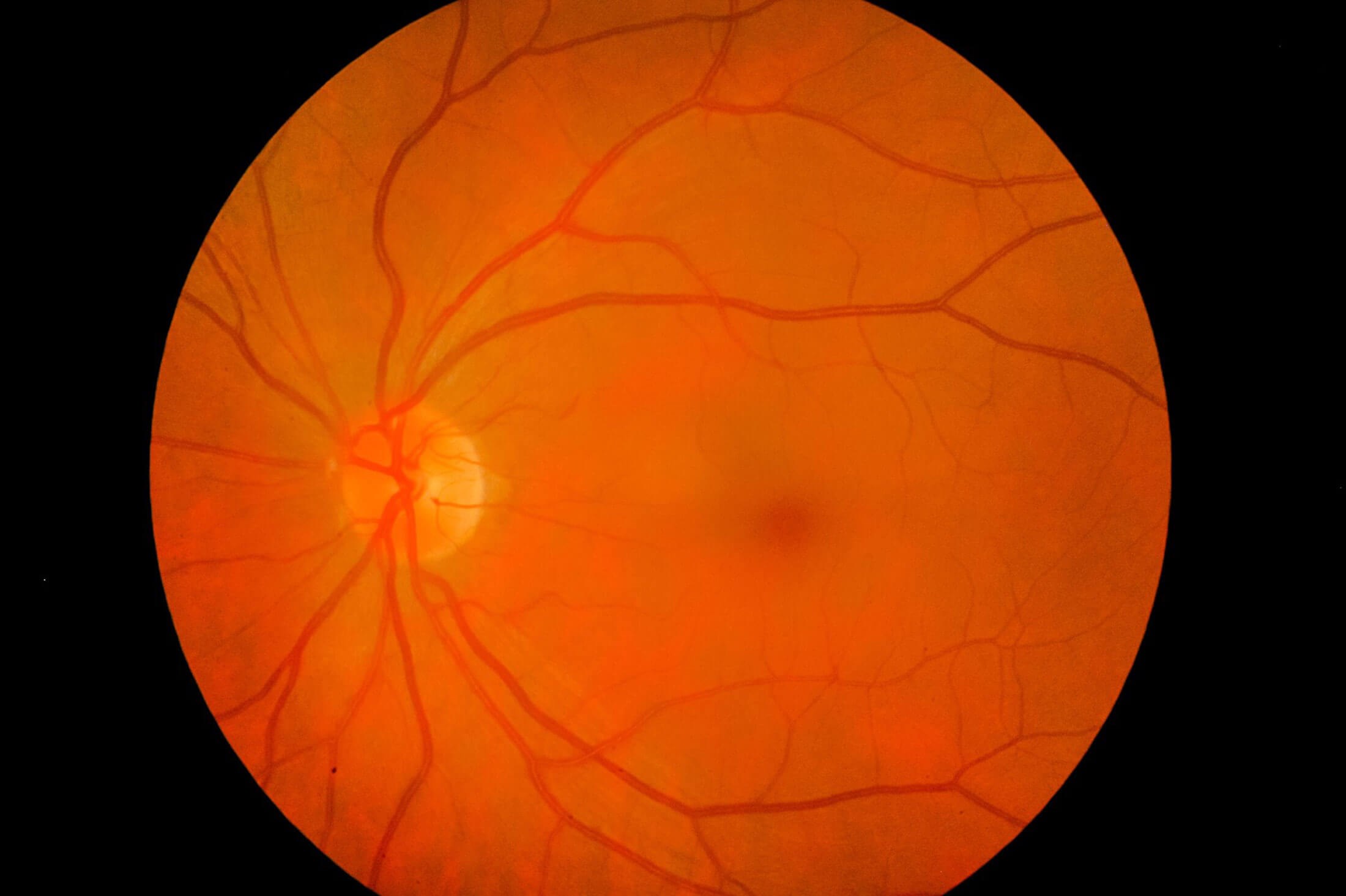
Figure 5: A normal retina [5].
References:
1. shutterstock.com/image-photo/young-girl-shows-chalazion-on-eyelid-746924596
2. https://www.shutterstock.com/image-vector/eye-stye-sty-problem-before-after-2109857147
3. https://www.shutterstock.com/image-photo/examination-treatment-patients-cataract-glaucoma-eyes-603714317
4. https://www.shutterstock.com/image-photo/close-corneal-ulcer-during-eye-examination-221926168
5. https://www.shutterstock.com/image-photo/medical-image-ocular-fundus-human-retina-1126908659
[All links last accessed January 2023].
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME







