
In recent years there has been a rapid expansion in a group of operations termed ‘minimally invasive’ or ‘micro invasive’ glaucoma surgery (MIGS). These options generally offer less significant IOP reduction, but with a more favourable safety profile when compared to traditional filtration surgery or aqueous shunt devices.
They have therefore become an attractive option in the right patient group. However, with an expanding list of surgical devices and operations available, it can be difficult to keep up. This article aims to summarise the more common options currently being used.
When to consider MIGS?
The majority of glaucoma surgeons still consider trabeculectomy to be the operation of choice for most patients with advanced disease who are at significant risk of vision loss in the short to medium term. However, we know there is a much vaster group of patients who may be on maximal medical management and would benefit from better IOP control, but who have less aggressive disease and an individual risk:benefit profile that may not yet justify trabeculectomy. It is these patients in which MIGS may be considered to either delay the need for more invasive surgery or prevent it from being required at all.
The other major consideration for MIGS is patients with glaucoma who are undergoing cataract surgery. We know that cataract surgery alone offers a certain reduction in IOP, but some MIGS procedures can be performed at the same time, offering further IOP reduction with minimal additional surgical time and risk.
What MIGS options are there?
Minimally invasive glaucoma surgery can be categorised by mechanism of action. Some MIGS options bypass the trabecular meshwork, some drain aqueous into the sub-conjunctival or suprachoroidal space, and some target the ciliary body [1]. Procedures may be performed ‘ab-interno’, meaning the approach is from within the eye, or ‘ab-externo’, meaning the approach is from outside the eye.
Trabecular meshwork bypass MIGS
There are a large number of trabecular meshwork bypass MIGS but some of the more commonly-used options include the iStent and the Hydrus Microstent. They are generally performed at the time of cataract surgery in patients with mild to moderate primary open angle glaucoma.
Figure 1: The iStent Inject, a hand-held injector capable of implanting two heparin-coated
titanium stents via a single corneal entry point. Figure courtesy of Glaukos.
iStent Inject
iStent Inject (see Figure 1) is a small device placed in the drainage angle that bypasses trabecular meshwork to allow aqueous fluid to drain directly from the anterior chamber into Schlemm’s canal. Two stents are typically implanted 2–3 hours apart, opposite the main corneal incision during cataract surgery.
Studies have shown that iStent in combination with phacoemulsification / IOL offers a 7.0mmHg reduction in IOP compared to 5.4mmHg in patients having phacoemulsification / IOL alone [2].
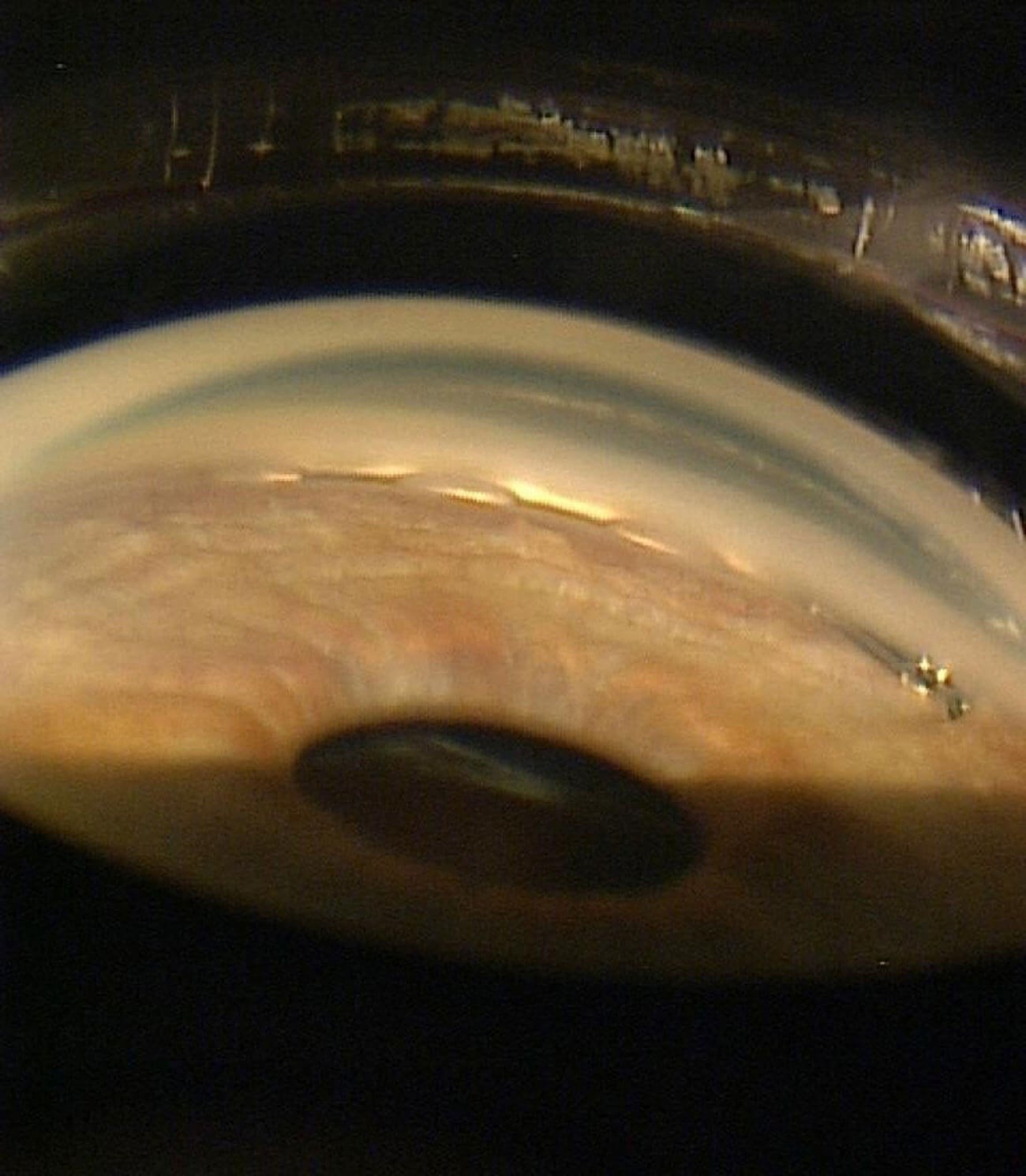
Figure 2: Hydrus Microstent in situ. Figure courtesy of Alcon.
Hydrus Microstent
The Hydrus Microstent (Figure 2) is an 8mm device inserted into Schlemm’s canal and spans 90 degrees of the drainage angle. It works through bypassing the trabecular meshwork, but it also acts as a scaffold to Schlemm’s canal. It can also be inserted using the same incisions made at the time of cataract surgery.
The HORIZON study showed that mean unmedicated IOP at two years reduced by 7.6mmHg in patients having Hydrus with phacoemulsification / IOL compared to 5.3mmHg in patients having phacoemulsification / IOL alone [3].
Trabecular meshwork resistance can also be overcome by incision or excision of the trabecular meshwork tissue. Procedures that utilise this include trabectome, gonioscopy assisted transluminal trabeculotomy (GATT), OMNI surgical system and Kahook dual blade goniotomy.
Sub-conjunctival MIGS
Devices such as the Xen stent and Preserflo Microshunt allow aqueous to drain from the anterior chamber into the sub-conjunctival space via a small tube. These devices are not always considered to be MIGS as they involve bleb-forming surgery and carry the risk of conjunctiva-associated complications. They may, however, offer a more favourable IOP reduction and therefore give options for patients with more moderate to severe disease.
Preserflo Microshunt
The Preserflo Microshunt is becoming an increasingly popular option. It is an 8.5mm-long tube inserted via an ab-externo approach. A superior peritomy is performed with a subtenons pocket formed and MMC applied. The device is then inserted through sclera into the AC. Once flow has been confirmed through the tube, the conjunctiva is closed to form a bleb. Battle, et al. found this offered a mean IOP reduction from 22.1 to 11.1mmHg as a standalone procedure [4].
Suprachoroidal MIGS
These devices target the uveoscleral outflow pathway to lower IOP and may be inserted ab-externo or ab-interno.
The ab-interno devices include the Cypass Microshunt and iStent Supra. Cypass was used for a number of years but was withdrawn from the market in 2018 as it was found to be associated with higher rate of endothelial cell count loss [1].
iStent Supra is a 4mm-long curved stent inserted ab-interno via a clear corneal incision. It is inserted with gonioscopic visualisation into the suprachoroidal space and can be done at the time of cataract surgery or as a standalone procedure. There is limited long-term data but one study has shown an IOP reduction of more than 20% and a reduction in the number of medications used in 98% of eyes [5].
Ab-externo suprachoroidal devices that have been used with varying success include the Gold Microshunt, Starflo, and Aquashunt.
Cycloablative MIGS – Endocyclophotocoagulation
Endocyclophotocoagulation (ECP) is a diode laser with a camera that enables endoscopic viewing. The ciliary processes are targeted over 200–360 degrees, aiming to blanch and contract the ciliary processes, reducing aqueous production.
One study found eyes having ECP with phacoemulsification had a mean IOP reduction from 18.1 to 16.0mmHg at two years. This was compared to a reduction from 18.1 to 17.3mmHg in the control group having phacoemulsification / IOL alone. Significantly fewer glaucoma medications were required in the treatment group at two years [6].
Summary
Minimally invasive glaucoma surgery bridges the gap between the medical management of glaucoma (and selective laser trabeculoplasty) and the potentially more major surgical options of trabeculectomy or tube surgery. From a patient perspective, there are clear benefits to the less-invasive nature of MIGS and the impact they may have on glaucoma control and medication burden. Whilst the extensive and ever-expanding list of MIGS gives the glaucoma surgeon an armoury of options, the challenge lies in not only when to offer MIGS, but which MIGS option to choose.
References
1. Wang J, Barton K. Overview of MIGS. In: Sng CCA, Barton K (Eds.). Minimally Invasive Glaucoma Surgery. Singapore; Springer Singapore; 2021:1–10.
2. Samuelson TW, Sarkisian Jr SR, Lubeck DM, et al. Prospective Randomized, Controlled Pivotal Trial of an Ab Interno Implanted Trabecular Micro-Bypass in Primary Open-Angle Glaucoma and Cataract: Two-Year Results. Ophthalmology 2019;126(6):811–21.
3. Samuelson TW, Chang DF, Marquis R, et al. A Schlemm canal microstent for intraocular pressure reduction in primary open-angle glaucoma and cataract: the HORIZON study. Ophthalmology 2018;126(1):29–37.
4. Batlle JF, Fantes F, Riss I, et al. Three-year follow-up of a novel aqueous humor microshunt. J Glaucoma 2016;25(2):e58–65.
5. Junemann A. Twelve-month Outcomes Following Ab Interno Implantation of Suprachoroidal Stent and Postoperative Administration of Travoprost to Treat Open Angle Glaucoma. 31st Congress of the European Society of Cataract and Refractive Surgeons. 5–9 October 2013; Amsterdam RAI, The Netherlands.
6. Francis BA, Berke SJ, Dustin L, Noecker R. Endoscopic cyclophotocoagulation combined with phacoemulsification versus phacoemulsification alone in medically controlled glaucoma. J Cataract Refract Surg 2014;40(8):1313–21.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME






