Award-winning* #KnowYourDrops eye drop compliance campaign helps patients for World Glaucoma Week to achieve medicines optimisation in ophthalmology.
The #KnowYourDrops campaign is fast becoming an internationally recognised model to help support healthcare professionals, with the provision of better tailored ophthalmic care, and patients, with the most effective administration and usage of ophthalmic treatments.
With poor ophthalmic medicine adherence largely being due to poor administration techniques, accompanied by poor treatment understanding, the award winning* #KnowYourDrops campaign was launched around six months ago to actively help break down barriers to poor compliance and to optimise medicines for those receiving eye drop treatment globally.
It is widely acknowledged that it is estimated between a third and a half of all medicines prescribed for long‑term conditions are not taken as recommended [1], including eye drops, so with National Institute of Health & Care Excellence (NICE) recently publishing guidance to manage medicines for adults receiving social care in the community [2], and the March parliamentary debate on preventing avoidable sight loss nationally, this timely article showcases how eye drop adherence has been progressively and successfully addressed at Moorfields Eye Hospital NHS Foundation Trust (Moorfields) so that the pharmacy-led initiative can be further integrated into care to benefit more patients.
Ophthalmic non-adherence and the benefits of support
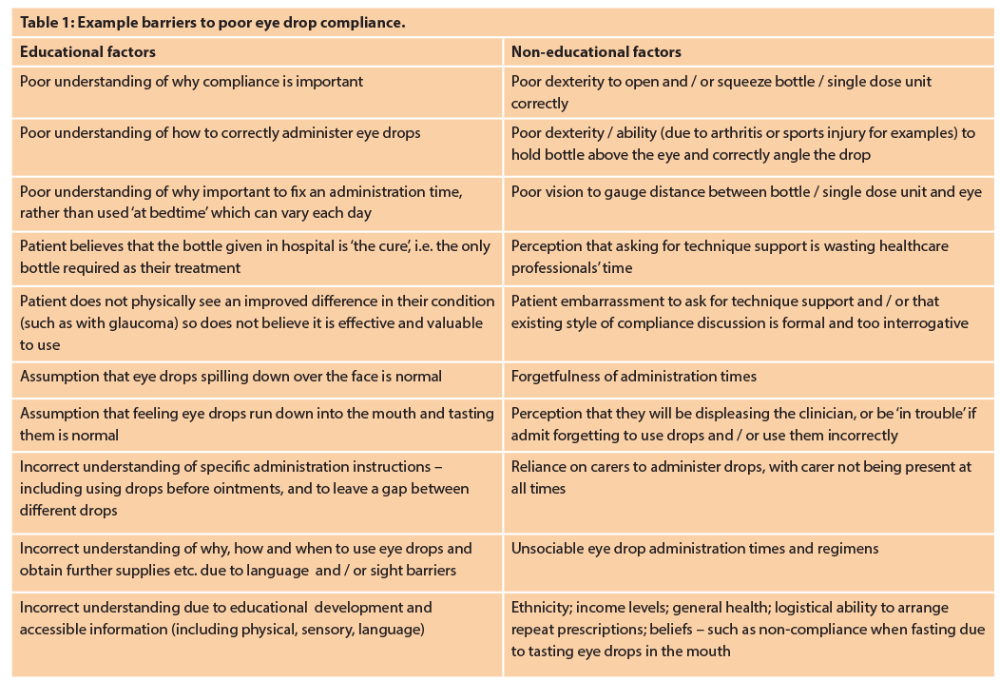
Aside from support on an educational level about treatment regimens, plans and patient concerns, support for correct eye drop technique and consideration of ophthalmic compliance aids is often overlooked outside specialist ophthalmic units. This type of treatment technique support differs widely when compared to other specialist medicines, for example, inhalers, where dedicated time is usually spent assessing, reviewing and continually supporting technique both in primary and secondary care. Eye drop technique support, however, is also essential, since treatment does not always improve sight (often a motivator to use drops correctly) but can prevent disease progression, such as glaucoma. Up to 50% of glaucoma patients are non-compliant with treatment [3] and given the consequences of treatment failure, it is vital to consider reasons for non-adherence and implement individualised measures of support to help overcome these barriers (Table 1). In turn, poor clinical outcomes, unnecessary polypharmacy and / or financial losses can be minimised, thus benefitting not only the patient / carer but also the NHS.
Although all Moorfields patients are reviewed and counselled on eye drop compliance and techniques, given the known facts about sight loss and proportion of glaucoma non-adherence, pharmacy and the clinical team decided to raise awareness of compliance and eye drop techniques, offer enhanced support to patients, carers and staff in order to reduce barriers for good compliance.
The International Glaucoma Association (IGA) greatly support this initiative and has provided direct support to this campaign, as well as additive support for all aspects of glaucoma care to all patients internationally.
Campaign format
#KnowYourDrops is a one-day advertised event at each Moorfields site, of which there are 32 spread across London, with advice and information on the trust’s website (www.moorfields.nhs.uk) and Twitter (@Moorfields) – including a useful online video (www.youtube.com/watch?v=BgodZZ2N2wY) and an opportunity to live-tweet compliance-related questions.

Engagement with local clinical commissioning groups, GPs, community partners and local eye networks through the clinic liaison officers helped to raise awareness and invitation. The consultant opens the session by speaking about compliance and eye drop techniques to all patients / carers, inviting everyone to talk to us for a review and advice. We integrate with the clinic team delivering a specialist pharmacist-led consultation, which features a medicine utilisation review, by assessing patients to achieve best techniques, raising awareness of compliance, and demonstrating compliance aids. We have an eye catching patient-facing stand with information, videos and compliance aids.
Patient / carer case studies
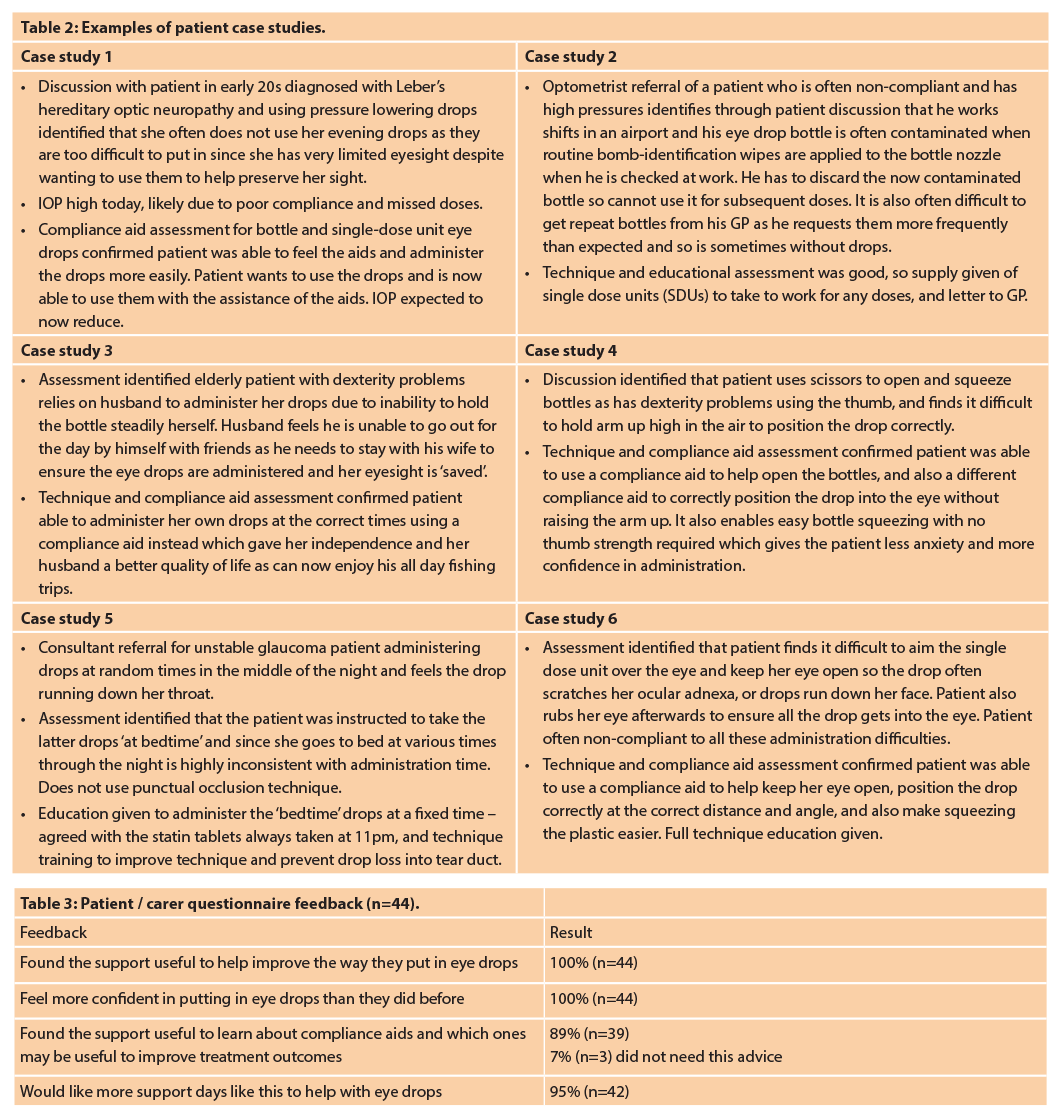
Numerous cases of improved medical care QOL, for patients as well as carers have been achieved, all varying in nature and addressing many non-adherence barriers (Table 2).
Patient / carer feedback
The presence of the campaign team assessing and supporting patients’ compliance was well received in all clinics, with exclusively positive comments collected from patients and carers associated with improved care and QOL (Figure 1).
Technique improvement
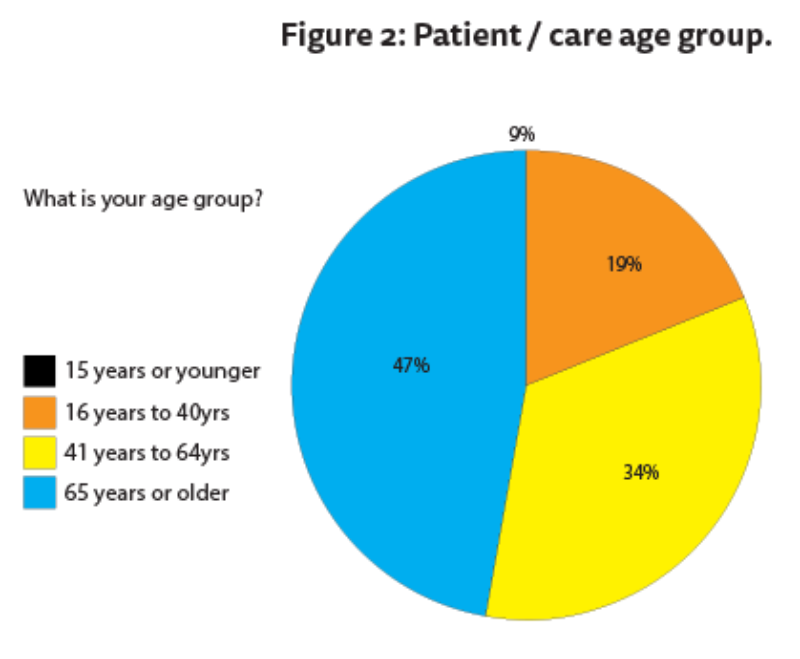
Patients / carers were invited to provide feedback about the support via a questionnaire (Table 3 and Figure 2). Data has so far been collected from five sites, with 95 feedback forms completed. All patients / carers (100%, n=95) expressed that the eye drop compliance support was useful to help improve the way they put in eye drops, and felt more confident in putting in eye drops than they did before. Almost half of those providing feedback were over 65 years of age (47%, n=45 Figure 2).
Compliance aid awareness
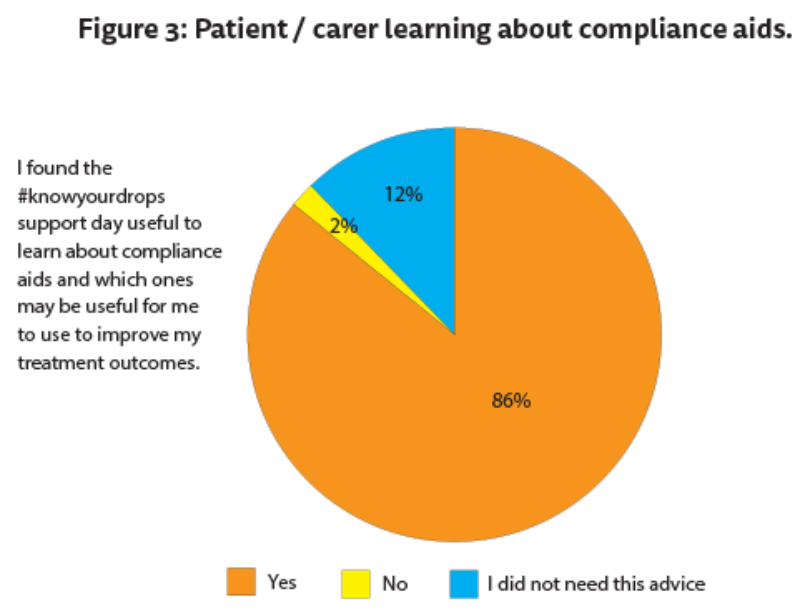
Almost all patients / carers (86%, n=82) said that they found the support day useful to learn about compliance aids and which ones may be useful to help improve treatment outcomes (Figure 3).
Additional specialist pharmacist-led Medicines Utilisation Review sessions
Almost all patients / carers (81%, n=81) said that they would like more support days like this to help with eye drops.
World Glaucoma Week 2017
In addition to regular #KnowYourDrops event days in clinics, the pharmacy team worked closely with the clinical team to support WGW17, and 12-18 March 2017 saw Moorfields fully engage with patients and carers throughout the week. With the ‘silent thief in the night’ affecting almost half a million patients in the UK [6], this was an opportunity to provide an intense week of the pharmacy-led medicines utilisation reviews for hundreds of patients and improve confidence and ability to use eye drop treatments, answer questions, improve quality of life and openly discuss any concerns about treatment regimens.
At the start of the week Moorfields provided a free patient information afternoon with two Moorfields consultant ophthalmologists hosting a patient seminar about glaucoma. They were joined by the #KnowYourDrops pharmacy team and the International Glaucoma Association presenting as part of the programme.
Discussion
The Public Health Outcomes Framework describes how health campaigns, building eye care pathways around the needs and experiences of patients, and improving concordance are essential to prevent sight loss [4]. Given the 2016 Royal National Institute for the Blind (RNIB) report estimating that more than 2 million people in the UK have sight loss [5], and that glaucoma is a leading cause of blindness in the UK with approximately 10% of UK blindness registrations being attributed to glaucoma [6], the #KnowYourDrops treatment review model strongly addresses these problems and helps this group of patients and their carers to improve treatment outcomes and quality of life (QOL). #KnowYourDrops also achieves NICE recommendations to support eye drop compliance in glaucoma patients [2]. The medication review is not, however, exclusive to this group of patients, and is applicable to all patients using ophthalmic medicines.
Successful eye drop technique
Treatment and care should take into account people’s needs and preferences [6], and as studies have found, there is not always a general relationship between medication adherence and the patients’ demographic data, clinical characteristics, or knowledge [7].
Eye drops are not always easy to administer, relative to oral dosing, including those given via multi-dose eye drop bottles. The inherent difficulties of delivering these medications have been reviewed in various studies [8,9], of which one has showed only 39% of patients with glaucoma administered the drops successfully.
With the numerous varied patient case studies already identified through this campaign (Table 2), it is apparent that a patient-specific approach is required to optimise adherence behaviour to eye drops, for new and existing patients and that there is not a one-size fits all training programme.
A patient-specific approach
To effectively break barriers (Table 1) to eye drop adherence, this campaign highlights that support must encompass a varied educational approach specific to each individual patient, and to involve any carers as relevant. It is inadequate to provide basic administration time counselling with a patient information leaflet, a poor quality demonstration and acceptance from the patient that they follow the correct technique and / or have been using eye drops ‘for years and know what they are doing’. Frequently throughout this campaign, new and existing patients have realised that they were not putting drops in correctly, had not understood the importance of fixed timings, and would have benefited from an aid but did not know they existed. Overall, the patients have benefitted from a tailored educational pharmacist-led consultation session.
Assessing techniques, identifying weaknesses, giving physical demonstrations with patients / carers practising and having guidance until they are comfortable with new advice, watching videos, worded and pictorial diagrams / leaflets, large font, translation services, speaking with other patients, and trying different devices with their own bottles are all methods used to help support patients. The patient-specific approach puts patients / carers at ease to engage in interactive conversations about compliance issues, which has often not yet been identified during their clinical pathway.
Repeated demonstrations have also helped overcome any educational barriers and establish correct understanding, since single sessions have been shown not to be as effective. According to one study, a single educational session on the proper use of topical drops was shown to improve the successful instillation of eye drops, however, it did not determine whether patients retain the improved instillation technique in the long-term or if the intervention only results in a short-term improvement [10].
Furthermore, ensuring that patients know why, how and when to use drops, and provision of information about their condition, consequences of not using the medications properly, and the adverse effects of the medication can result in low adherence to glaucoma treatment [11], and are all included in the pharmacy-led #KnowYourDrops medicine review.
Improved quality of life for patients and carers
In many cases, the relatively simple intervention (without complex medical equipment / machines or diagnostic reagents for examples) of spending sometimes only 10-15 minutes to assess technique and encourage open and honest interactive discussion about adherence has not only helped improve clinical outcomes, but also improved QOL – often providing feelings of independence, confidence, self-satisfaction, calmness and dignity. Some patients require longer sessions such as half an hour, or repeated sessions throughout their outpatient appointment, and perhaps some also include clinician involvement. It is fair to say, however, that in all cases quality of life has been improved in some way as a result of the targeted adherence review either for themselves or their carer.
According to one study, 17% of patients relied on another person to administer the drops [8], where poor manual dexterity and reduced vision often worsened the administration problems. The campaign hopes to raise healthcare professionals’ awareness that it is not always just the patient who benefits, as it is often the carer, by lessening the burden and constraints of being relied upon to administer eye drops for family members multiple times a day. In several cases, when the carer is away there is no practical contingency for eye drop administration, and so doses are missed which can ultimately affect the condition, however, this can be avoided with suitable administration support.
Role of the pharmacist
This campaign highlights that medicines optimisation in ophthalmology is often an overlooked area without direct actions being taken, and requires professional awareness, skills and knowledge to be able to better provide support across all patient groups. Most of the population will use eye drops at some stage in their lives such as hay fever, infection or dry eye, and it is often assumed that basic counselling about drop frequency and a quick check that patients know how to use eye drops is sufficient for all patients. However, with 50% of all glaucoma patients being non-compliant with treatment [3] and 10% of UK blindness registrations attributable to glaucoma [6], it is clear that this is an area where pharmacists can help make a positive difference using their underpinning pharmaceutical knowledge. With glaucoma being the second leading cause of blindness globally [12], the assessment of a patient’s ability to administer eye drops correctly should be a routine part of the glaucoma examination. At the very least this needs to be an integral part of each pharmacist counselling session, whether in primary or secondary care, and it has been commented on by patients during this campaign that this supportive care is “lacking in the system and is so valuable and necessary.”
Studies have shown that regular monitoring can help to ensure that the information has been retained [10] by the patient. Pharmacists are ideally placed to improve eye drop compliance within the hospital as well as the community setting. However, few are actively providing this role and nurses are sometimes expected to provide this additive care often outside the scope of expert ophthalmic medicines knowledge. According to one study, 63% of patients were given advice about instillation technique, of which these 5.3% received this by a hospital pharmacist, and 2% from a community pharmacist [13].
Savings to the NHS
There are over a million glaucoma-related outpatient visits in the hospital eye service annually [6], which could potentially be avoided with reviews such as the #KnowYourDrops clinics which help prevent non-adherence and improve treatment outcomes, thus preventing unnecessary appointments.
In addition, several patients use excessive drops unnecessarily purely due to poor administration techniques, which adds to the burdens of repeat prescribing and national medication costs.
By better supporting ophthalmic adherence, with pharmacy-led medicines utilisation reviews, this not only improves treatment outcomes and QOL, but also helps to reduce pressures across the NHS by saving time and money.
Conclusion
Ophthalmic non-adherence should not be seen as the patient’s problem [1] and should be part of healthcare delivery at every level to address and support the patient. In addition, an important part of poor adherence is an incorrect dosing technique [10], and healthcare professionals can reduce both educational and non-educational potential barriers to ophthalmic non-adherence for all patients. However, potential time, knowledge and skills amongst the profession to do this effectively are sadly often lacking.
This campaign marks a landmark in what could potentially be a routine part of every ophthalmic patients’ pathway in that patients are reviewed by a dedicated pharmacist in the outpatient clinic setting for medicines adherence for better treatment outcomes, improved QOL and reduced subsequent financial burden on the NHS through reduced eye drop supplies and hospital / GP appointments.
Medicines utilisation reviews are carried out frequently in community pharmacies by accredited pharmacists undertaking structured adherence-related reviews, however, there is no national target group for ophthalmology and this practice is not currently nationalised throughout the NHS. The next stage of the campaign is to achieve official research findings as a before and after pilot study to evaluate the clinical efficacy and patient reported outcome measures of the pharmacist-led medication utilisation reviews in patients using drops for ocular hypertension / glaucoma in outpatient clinics. The results will then allow further research to support implementing this model at national level.
Given that sight loss is costing over £28 billion to the UK economy [5], the results of the research following this excellent innovative initiative will really help address this issue and it is expected that practice will change nationally in light of the #KnowYourDrops campaign findings.
In conclusion, since its launch six months ago the double-award winning* #knowyourdrops eye drop adherence campaign successfully helps achieve medicines optimisation in ophthalmology, and has been integrated and rolled out throughout the Moorfields network. We look forward to learning how the initiative expands in 2017, including the results from research studies.
* #KnowYourDrops has achieved the Hospital Pharmacy Europe People’s Choice Award, and recently the respected Moorfields Eye Hospital Charity Award for Innovation, Research or Education.
References
1. Medicines adherence: involving patients in decisions about prescribed medicines and supporting adherence. Clinical guideline [CG76].
2. Managing medicines for adults receiving social care in the community NICE guideline [NG67].
3. Johnson MRD, Cross, Scase MO, et al, 2012. A review of evidence to evaluate effectiveness of intervention strategies to address inequalities in eye health care. RNIB and De Montfort University.
4. Public Health Outcomes Framework 2013-2016 Healthy lives, healthy people: Improving outcomes and supporting transparency: Public Health England.
5. RNIB, The State of the Nation Eye Health 2016.
6. NICE (2009) Glaucoma: diagnosis and management. NICE clinical guideline 85. Available at
www.nice.org.uk/CG85 [NICE guideline].
7. Ulrich Welge-Lussen et al, 2014. Assessing the adherence behaviour of glaucoma patients to topical eye drops. Patient Preference and Adherence.
8. Hennessy AL, Katz J, Covert D, et al. A video study of drop instillation in both glaucoma and retina patients with visual impairment. Am J Ophthalmol 2011;152(6):982-8.
9. Marston MV. Compliance with medical regimens: a review of the literature. Nurs Res 1970;19(4):312-23.
10. Lazcano-Gomez G, Castillejos A, Kahook M, et al. Video-graphic Assessment of Glaucoma Drop Instillation. J Curr Glaucoma Pract 2015;9(2):47-50.
11. Friedman DS, Hahn SR, Gelb L, et al. Doctor-patient communication, health-related beliefs, and adherence in glaucoma results from the Glaucoma Adherence and Persistency Study. Ophthalmology 2008 Aug;115(8):1320-7.
12. WHO (2004). World Health Organization. Programmes. Bulletin of the World Health Organization. Volume 82, Number 11, November 2004, 811-90.
13. Watson SL, European Society of Ophthalmology. 2001.
TAKE HOME MESSAGE
-
Successful ophthalmic treatment relies on effective drug administration and all patients, regardless of previous eye drop therapy or length of treatment, benefit from an assessment of correct technique and potential barriers to achieve maximum therapeutic benefit.
-
>50% patients with glaucoma, an asymptomatic disease and a leading cause of sight-loss, are non-compliant with using eye drops.
-
Educating and engaging patients and carers about why, how and when to use their eye drops is essential to support medicines optimisation, all of which can be delivered by the pharmacy team as well as by clinicians and nursing staff.
-
Support for eye drop compliance not only supports medicines optimisation but often significantly improves QOL for patients and carers by, for example, improving confidence, providing patient independence, improving patient experience and personal management of their condition, reducing reliance of carers to administer drops, and alleviating any stresses and operational burdens associated with using carers.
-
Pharmacists can support the clinical team by delivering a specialist pharmacist-led consultation and medicine utilisation review for all patients at the initial stages of therapy and along the patient treatment pathway, to provide continuous support throughout the treatment course and prevent non-adherence. Routine counselling of repeat eye drops is a valuable opportunity to check technique and offer advice to improve this, and to ensure maximum benefit from treatment.
COMMENTS ARE WELCOME