Modern cataract surgery aims to provide patients with the best possible visual outcome with the least dependence on spectacles and minimal or no complications and to treat both cataract and refractive errors with a single procedure.
Phacoemulsification is the standard surgical technique with implantation of a monofocal intraocular lens (IOL). This article reviews recent published research evaluating IOL implant technology designed to extend and improve refractive performance following cataract extraction, including trifocal IOLs, extended depth of focus multifocal IOLs, and shape-changing accommodating IOLs being tested in clinical development.
Toric IOL options offer distance vision without glasses for patients with pre-existing astigmatism
Astigmatism following cataract surgery is an important cause of suboptimal uncorrected distance visual acuity (UDVA) and need for distance spectacles. Toric IOLs may correct for pre-existing corneal astigmatism at the time of cataract surgery and have been shown to result in increased unaided distance visual acuity [1].
A systematic review and meta-analysis of 13 randomised clinical trials found that implantation of toric IOLs during cataract surgery is associated with significantly better postoperative UDVA, greater spectacle independence, and lower amounts of residual astigmatism than non-toric IOLs even when relaxing incisions were made [2]. For the included studies, with postoperative follow-up of three to six months, 70.3% of patients reported that they never required spectacles for distance viewing after toric IOL implantation compared with 46.8% in the non-toric IOL groups with and without a relaxing incision. Most of the studies used the Acrysof Toric IOL (Alcon), with some studies using the Mflex-T multifocal IOL (Rayner), the Lentis Unico (Oculentis), or the Tecnis toric IOL (Abbott Medical Optics). Both the toric and non-toric IOL were multifocal in one study. Study authors recommended toric IOL implantation for cataract patients with regular corneal astigmatism who want postoperative spectacle independence for distance viewing.
Chang et al. reported visual performance results after bilateral implantation of AT LISA (Carl Zeiss Meditec) 909M, a four-haptic diffractive toric multifocal IOL, in high myopes [3]. Ten (71%) of 14 patients reported complete spectacle independence, with good visual performance and high patient satisfaction overall in high myopes (axial length of ≥26mm and corneal astigmatism of >1 dioptre [D]). A prospective study by Kretz and colleagues reported effective restoration of the distance, intermediate and near vision after cataract surgery with good levels of visual quality and minimal photic phenomena in eyes undergoing cataract surgery with implantation of the trifocal toric IOL AT LISA tri toric 939MP [4].
Precizon Toric (Ophtec) is a hydrophilic acrylic, monofocal aspheric IOL, with a transitional conic toric surface, designed to be more tolerant of misalignment. A prospective study evaluated outcomes and rotational stability of the Precizon toric IOL for the correction of pre-existing corneal astigmatism in cataract surgery, involving 40 eyes of 27 patients with corneal astigmatism greater than 1.0 D. The median postoperative UDVA was better than preoperative best-spectacle corrected distance VA (0.02 logMAR vs 0.19 logMAR), and postoperative UDVA at six months’ follow-up was 0.1 logMAR or better in 95% of the eyes [5]. No cases required IOL realignment.
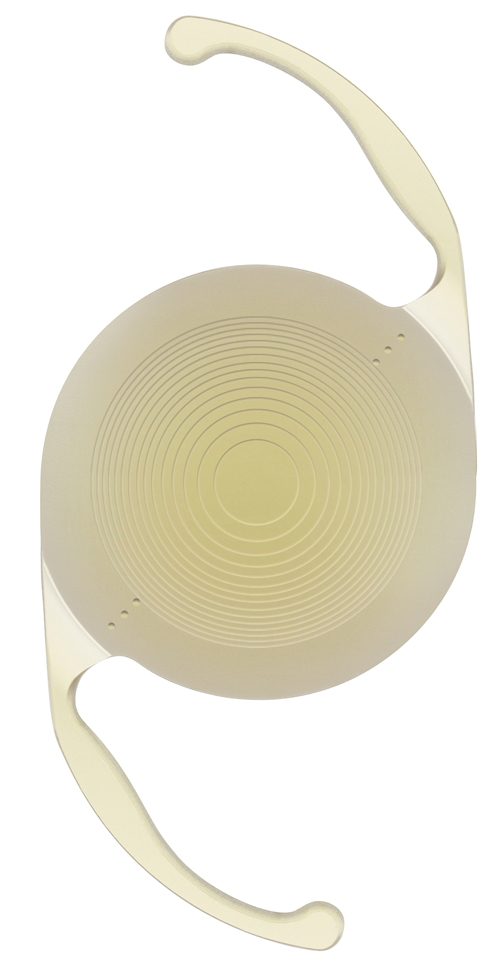
Figure 1: Investigational FluidVision Accommodating Intraocular Lens
(image courtesy of PowerVision Inc.)
Multifocal IOL selection: still a trade-off between visual symptoms and quest for spectacle independence?
Multifocal IOLs are effective at improving near vision without any adverse effect on distance VA, but have been associated with reduced contrast sensitivity and increased risk of perception of halos [6]. A review of multifocal versus monofocal IOLs after cataract extraction concluded that multifocal IOLs are effective at improving near vision relative to monofocal IOLs, with more frequent freedom from use of glasses with multifocal than monofocal IOLs [6]. Whether these benefits outweigh the adverse effects of multifocal IOLs will vary between individual patients. A randomised, multicentre clinical trial of multifocal versus monovision IOLs after bilateral cataract surgery found greater spectacle independence with a diffractive multifocal IOL than the monofocal implant (71.3% vs. 25.8%), but a greater likelihood of IOL exchange in the first postoperative year with the multifocal IOL (5.7% vs. none in the monovision arm) [7].
A double-masked, prospective, randomised, controlled clinical trial by the Moorfields IOL Study Group evaluated visual symptoms and spectacle freedom after bilateral multifocal IOL implantation with either the AT LISA 809M IOL or ReSTOR SN6AD1 (Alcon Laboratories) [8]. Both diffractive bifocal IOLs produced high levels of spectacle independence (77.6% and 82.1% for ReSTOR SN6AD1 and AT LISA 809M, respectively), with halo the most prominent dysphotopsia symptom, reported as very bothersome by 6% in both IOL groups. Defining the trade-off between visual symptoms and spectacle independence is a central issue in the evaluation of multifocal IOLs, noted Allan and colleagues for the Moorfields IOL Study Group.
Moore et al. reviewed recently published studies reporting postoperative outcomes of rotationally asymmetric multifocal IOLs [9]. Use of these IOLs has been shown to achieve excellent visual and refractive outcomes, with reduced photopic phenomenon such as glare and halos leading to better patient satisfaction. Greenstein and Pineda, having reviewed literature comparing multifocal IOL implantation with pseudophakic monovision to treat presbyopia, observed that both multifocal IOLs and monovision appear to address presbyopia with a high level of patient satisfaction [10]. While complete spectacle independence is higher with multifocal IOLs, more glare and halos were reported by multifocal IOL patients [10].
Newer-generation trifocal IOL solutions
Newer trifocal IOLs have been developed with the aim of providing functional intermediate visual acuity. The Acrysof IQ PanOptix (Alcon) trifocal IOL, which received Conformité Européenne (CE) mark approval in June 2015, is designed to improve near to intermediate vision, in addition to providing excellent distance vision, and increase independence from glasses. Without presbyopia-correcting IOLs, most patients undergoing cataract surgery experience compromised near vision often requiring additional vision correction following surgery such as reading glasses or contact lenses. The Acrysof IQ PanOptix trifocal IOL is indicated for adult patients with and without presbyopia undergoing cataract surgery who desire near, intermediate and distance vision with increased spectacle independence.
The FineVision IOL (Physiol) features a diffractive trifocal optic, combining two diffractive structures that are adjusted to offer the +3.5 D addition for near vision and +1.75 D addition for intermediate vision. Designed to reduce the loss of light energy resulting from any diffractive system, the energy gain results in a significantly improved performance for intermediate vision while maintaining the performance for far and near vision. The FineVision optic has a diffractive anterior surface entirely convoluted. By varying the height of the diffractive step, the amount of light distributed to the near, intermediate and distant foci is adjusted according to the pupil aperture. Visual results obtained with the FineVision optic show very satisfactory uncorrected VA at all distances and an extended range of vision in all light conditions.
Kohnen and colleagues evaluated visual and refractive outcomes after bilateral implantation of a trifocal IOL (AT LiSA tri839MP) in 27 patients (54 eyes) [11]. At three months following surgery, mean spherical equivalent was 0.05±0.32 D, with good VA of 0.1 logMAR or better at far, intermediate, and near distance, and high spectacle independence. Binocular uncorrected VA was -0.1 ± 0.1 logMAR or about 20/16 at distance, and 0.0 ± 0.1 logMAR or 20/20 at intermediate and near distances. Moreover, contrast sensitivity was within normal range in photopic, mesopic and mesopic with glare conditions. Despite optical phenomena, with halos the most common, patient satisfaction was high at 92%. Reducing the intermediate range dip in VA while maintaining near vision adequate for reading in most patients gives trifocal IOLs an advantage over bifocal or extended-depth-of-focus designs, according to investigators.
A meta-analysis of peer-reviewed studies of multifocal IOL implantation in presbyopic patients with cataract or having refractive lens exchange found the mean postoperative monocular UDVA was 0.05 logMAR ± 0.006 (SD) (Snellen equivalent 20/20) in 8797 eyes [12]. The mean binocular UDVA was 0.04 ± 0.00 logMAR (Snellen equivalent 20/20), with a mean spectacle independence of 80.1%, in 6334 patients [12].
Comparative optical bench performance tests show the optimum intermediate image was at 60cm for the Acrysof IQ PanOptix (+2.17 D/+3.25 D IOL) and 80cm for the AT LISA Tri 839MP (+1.66 D/+3.33 D IOL) and FineVision Micro F (+1.75 D/+3.50 D IOL) [13]. Better intermediate vision at 60cm is preferred for everyday tasks such as computer work, noted study authors from Alcon Research [13]. The PanOptix trifocal IOL showed equivalent or better performance in image quality, resolution and photic phenomena compared with the other two trifocal IOLs. Another in vitro bench evaluation compared the optical characteristics of the PanOptix presbyopia-correcting trifocal IOL and the multifocal Acrysof IQ ReSTOR +3.0D IOL [14]. The PanOptix IOL showed better resolution and image quality performance at the intermediate focus than the ReSTOR +3.0 D IOL, with comparable resolution and image quality performance in distance and near foci. The halo propensity for PanOptix was slightly higher than that for ReSTOR +3.0D IOL.
The SBL-3 Segmented Bifocal Lens (Lenstec), a rotationally asymmetric / segmented multifocal IOL, is a presbyopic lens that is designed to improve contrast sensitivity, minimise halos and glare, and provide superior near, intermediate and distance vision compared with other presbyopic IOLs following cataract removal. The SBL-3 comes with a true 3.0D sector-shaped add with a seamless transition zone between the distance and near segments, and is available in 0.25 D power increments. Results from several prospective studies evaluating the performance of the SBL-3 note a high level of near, intermediate and distance vision, very limited amounts of visual side-effects, and extremely high patient satisfaction and spectacle independence ratings. The SBL-3 lens is currently being evaluated in a US Food and Drug Administration (FDA) one-year clinical trial that includes a control arm implanted with a monofocal IOL.
Figure 2: AcrySof IQ PanOptix Toric Presbyopia-correcting IOL.
Figure 3: AcrySof IQ PanOptix Presbyopia-correcting IOL.
Extended range of vision IOLs
The Tecnis Symfony IOL (Abbott Medical Optics), CE mark approved in June 2014, is an extended depth of focus (or extended range of vision) IOL providing an option for patients that may result in better vision across a broader range of distances. Traditional monofocal IOLs improve distance vision, while the Tecnis Symfony IOL improves visual acuity at close, intermediate and far ranges and may reduce the need for contact lenses or glasses after cataract surgery.
Approval of the Symfony IOL by the US FDA in June 2016 was based on results from a randomised clinical trial comparing 148 cataract patients implanted with the Tecnis Symfony IOL to 151 cataract patients implanted with a monofocal IOL, who were followed for six months after implantation. For the group implanted with the Tecnis Symfony IOL, 77% had good vision (20/25), with glasses at intermediate distances, compared with 34% of those receiving the monofocal IOL. For near distances, patients in the Tecnis Symfony IOL group were able to read two additional lines on the ETDRS chart than those with the monofocal IOL. Results from an international multicentre study across 40 clinical sites in Europe found that the extended range of vision IOL provided successful vision restoration across all distances after cataract surgery, with spectacle independence achieved in 85% in a prospective cases series of 411 patients [15]. At four to six months after cataract surgery, the mean decimal uncorrected distance, intermediate and near visual acuities were 0.95, 0.81 and 0.69, respectively. More than 90% of patients reported no or mild halos, glare, starbursts or other photic phenomena.
The small-aperture IC-8 IOL (AcuFocus), CE mark approved in 2014, is a one-piece hydrophobic acrylic lens with an embedded opaque annular mini-ring with a central aperture, designed to provide a range of vision across various distances for patients with cataracts, extending depth of focus by combining small aperture technology with a monofocal lens. A prospective case series found that all eyes (n=12) implanted monocularly with the IC-8 IOL maintained 20/40 or better VA over a range of +0.50 D to -1.50 D of defocus over 12 months postoperatively [16]. Mean monocular uncorrected distance, intermediate, and near visual acuities improved significantly from 0.42±0.18, 0.52±0.22 and 0.66±0.23 preoperatively to 0.06±0.08 (P<.0001), 0.07±0.11 (P<.0001), and 0.11±0.15 (P<.0001) at one month, respectively, and remained stable through 12 months. According to the manufacturer, IC-8 IOL provides a full range of vision without resulting in a loss of far vision when the target refraction is achieved, and delivers excellent image resolution across a broader through-focus range of vision with better image contrast and without ghosting symptoms as compared to other premium lenses.
Another means of extending depth of focus is to induce spherical aberration in the lens, for example using light-adjustable IOLs.
The Light Adjustable Lens (Calhoun Vision) is an investigational device currently being evaluated in clinical trials. The IOL consists of ultraviolet-sensitive silicone polymers that allow spherical and toric adjustment as well as correction of aberrations using a special lamp, providing a customised solution that delivers the right combination of spherical aberration and defocus correction for individual patients. Villegas and colleagues found that controlled amounts of negative spherical aberration and defocus can be induced in eyes implanted with adjustable intraocular lenses to enhance near vision [17].
The WIOL-CF (Wichterle IOL – Continuous Focus) from Medicem is a bioanalogic IOL incorporating proprietary biocompatible material and designed to provide polyfocal accommodation within a continuous range from near to distant focus for improved vision without further correction. The haptics-free IOL is almost 9mm in diameter, with large, glare-free optics to ensure undisturbed night and peripheral vision, small incision size and marked by a low incidence of posterior capsule opacification. Long-term follow-up results, with average postoperative follow-up of 5.6 years (range two-nine years, n=40), show a patient-satisfaction rate of 97% and binocular uncorrected VA for far, intermediate and near VA of 0.01 logMAR, 0.12 logMAR and 0.36 logMAR, respectively [18].
Shape-changing accommodating IOLs in clinical development
Alcon and US-based PowerVision struck a strategic alliance last year to focus on developing and commercialising fluid-driven accommodating IOLs for cataract patients. The fluid-based technology represents what Alcon called a potential game-change in the category with the promise to offer patients a natural, continuous range of near to far vision. Alcon’s investment will fund further development and clinical trials, as well as provide Alcon the option to acquire PowerVision.
An investigational FluidVision fluid-driven accommodating IOL (AIOL) (PowerVision Inc.) being evaluated in single-centre and multicentre clinical studies aims to mimic the eye’s natural accommodative process. The FluidVision AIOL is the first true shape-changing IOL designed for clear vision from near to distance and anywhere in between. The FluidVision AIOL utilises the eye’s natural accommodative forces to reshape the anterior surface of the lens to change optical power. It does this by using a proprietary hydraulic mechanism to drive fluid from the periphery of the device to the central lens portion and back again, changing the curvature of the lens surface and facilitating accommodation. The act of accommodation forces fluid from the haptics into the optic thereby increasing thickness and optical power. During disaccommodation fluid flows back into the haptics.
The current fourth-generation FluidVision lens requires an incision size of 3.5mm, with study results showing excellent, stable outcomes with proven accommodative function without compromising capsular bag integrity or clarity. Nearly 150 patients in clinical studies in South Africa and Europe have been implanted with the FluidVision AIOL. Study results demonstrate excellent and stable monocular and binocular VA at distance, intermediate and near through 36 months. Amplitude of accommodation was stable at 3.3 D monocular and 3.9 D binocular [19]. Pipeline developments include FluidVision 20/20, a lens designed to provide twice the accommodation and give 20/20 vision across all distances. Initial bench testing results suggest this new lens can provide greater crisper vision than even the most advanced multifocals from 0.0 D to 3.0 D of accommodation. Other product developments targeted include smaller incision size, a toric model and then post-implant adjustment.
Elsewhere, Elenza is developing an electroactive Sapphire AutoFocal IOL that uses a proprietary combination of liquid-crystal chemistry, electricity and integrated-circuitry to create smart optics. The technology includes an electro-active switchable element that automatically adjusts focusing power electronically to maintain constant in-focus vision for various working needs and / or light environments. The lens, controlled by a micro-sized power cell with an expected 50+ year rechargeable cycle life, is fully programmable and customisable after implantation.
The sulcus-positioned AkkoLens Lumina accommodative IOL (AkkoLens International) utilises two shifting optical elements to achieve accommodation. The natural muscle of the eye shifts the optical elements to provide sharp images at a distance and nearby for spectacle-free vision. One-year results, from a randomised clinical trial that included a control group of eyes implanted with an Acrysof SA60AT monofocal IOL, demonstrate that the Lumina accommodative IOL effectively restores visual function, accommodation and contrast sensitivity after cataract surgery [20]. Defocus curves showed a statistically significant difference between groups for defocus ranging from -4.50 to -0.50 D (P <0.01) with significantly higher visual acuities for the Lumina group.
Closing comments
Trifocal diffractive multifocal IOLs are gaining widespread traction amongst UK cataract and refractive surgery practices, and are considered to have the edge over other lens implant options with regard to spectacle freedom. There is also considerable interest in the use of bifocal IOLs with a low refractive addition (+1.0-1.5 D) as an enhanced micro-monovision solution, the main driver here being the desire to provide an enhanced range of unaided focus whilst minimising dysphotopsia side-effects. Both these modalities appear to have fewer visual quality issues than earlier generation multifocal IOLs. The overall direction of travel in IOL research and technology development is continuing refinement towards even better lens designs with fewer photopic side-effects and improved rates of patient satisfaction. And thereby achieve more predictable surgical outcomes.
References
1. Agresta B, Knorz MC, Donatti C, Jackson D. Visual acuity improvements after implantation of toric intraocular lenses in cataract patients with astigmatism: a systematic review. BMC Ophthalmol 2012;12:41.
2. Kessel L, Andresen J, Tendal B, et al. Toric intraocular lenses in the correction of astigmatism during cataract surgery: a systematic review and meta-analysis. Ophthalmology 2016;123(2):275-86.
3. Chang JS, Chan VK, Ng JC, Law AK. Visual performance after bilateral implantation of a four-haptic diffractive toric multifocal intraocular lens in high myopes. J Ophthalmol 2016;2016:5320105.
4. Kretz FT, Breyer D, Klabe K, et al. Clinical outcomes after implantation of a trifocal toric intraocular lens. J Refract Surg 2015;31(8):504-10.
5. Vale C, Menezes C, Firmino-Machado J, et al. Astigmatism management in cataract surgery with Precizon(®) toric intraocular lens: a prospective study. Clin Ophthalmol 2016;10:151-9.
6. Calladine D, Evans JR, Shah S, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev 2012;(9):CD003169.
7. Wilkins MR, Allan BD, Rubin GS, et al; Moorfields IOL Study Group. Randomized trial of multifocal intraocular lenses versus monovision after bilateral cataract surgery. Ophthalmology 2013;120(12):2449-55.
8. Maurino V, Allan BD, Rubin GS, et al; Moorfields IOL Study Group. Quality of vision after bilateral multifocal intraocular lens implantation: a randomized trial--AT LISA 809M versus AcrySof ReSTOR SN6AD1. Ophthalmology 2015;122(4):700-10.
9. Moore JE, McNeely RN, Pazo EE, Moore TC. Rotationally asymmetric multifocal intraocular lenses: preoperative considerations and postoperative outcomes. Curr Opin Ophthalmol 2017;28(1):9-15.
10. Greenstein S, Pineda R 2nd. The quest for spectacle independence: a comparison of multifocal intraocular lens implants and pseudophakic monovision for patients with presbyopia. Semin Ophthalmol 2016:1-5. [Epub ahead of print]
11. Kohnen T, Titke C, Böhm M. Trifocal intraocular lens implantation to treat visual demands in various distances following lens removal. Am J Ophthalmol 2016;161:71-7.
12. Rosen E, Alió JL, Dick HB, et al. Efficacy and safety of multifocal intraocular lenses following cataract and refractive lens exchange: meta-analysis of peer-reviewed publications. J Cataract Refract Surg 2016;42(2):310-28.
13. Carson D, Xu Z, Alexander E, et al. Optical bench performance of 3 trifocal intraocular lenses. J Cataract Refract Surg 2016;42(9):1361-7.
14. Lee S, Choi M, Xu Z, et al. Optical bench performance of a novel trifocal intraocular lens compared with a multifocal intraocular lens. Clin Ophthalmol 2016;10:1031-8.
15. Cochener B; Concerto Study Group. Clinical outcomes of a new extended range of vision intraocular lens: international multicenter Concerto Study. J Cataract Refract Surg 2016;42(9):1268-75.
16. Grabner G, Ang RE, Vilupuru S. The small-aperture IC-8 intraocular lens: a new concept for added depth of focus in cataract patients. Am J Ophthalmol 2015;160(6):1176-84.
17. Villegas EA, Alcón E, Mirabet S, et al. Extended depth of focus with induced spherical aberration in light-adjustable intraocular lenses. Am J Ophthalmol 2014;157(1):142-9.
18. Mazal Z, et al. Long term results of WIOL-CF® intraocular lens implantation. Presented at the Congress of Czech Society of Refractive and Cataract Surgery, Ostrava 5/2014.
19. Roux P, Potgieter F. Thirty-six month monocular and 12-month binocular experience with a fluid-filled accommodative intraocular lens. Paper presentation at the XXXIV Congress of the ESCRS, 10-14 September 2016, Copenhagen, Denmark.
20. Alio JL, Simonov A, Plaza-Puche AB, et al. Visual outcomes and accommodative response of the Lumina accommodative intraocular lens. Am J Ophthalmol 2016;164:37-48.
COMMENTS ARE WELCOME