Despite being the most common cause of painful orbital mass in adults and the third most common orbital disease, orbital inflammatory syndrome still proves to be a difficult ocular condition to diagnose, treat, and manage.
A 41-year-old lady presented to the Emergency Department of our District General Hospital in the early hours of a sweltering July summer’s day. With no comorbidities, no ocular history and previously bilateral 6/5 vision, she reported to have developed a left-sided abrupt-onset severe peri-orbital swelling and ocular pain overnight, as she slept.
Ophthalmology was contacted for an urgent review and on further inspection, a complete ptosis, proptosis, conjunctival chemosis and hyperaemia in the same eye were found. Of note was a small, red, pruritic patch – resembling a graze – on the medial aspect of the upper lid; only this area was tender on palpation. She was systemically well with no recent history of fever, infection or injury. Further ophthalmic examination also revealed a complete ophthalmoplegia, relative afferent pupillary defect (RAPD) and, devastatingly, a new visual acuity of no perception to light (NPL) in the left eye. Central retinal artery occlusion (CRAO) was seen on fundoscopy.
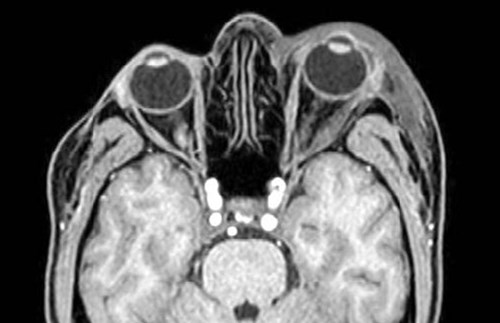
Figure 1. MRI Orbit with contrast both. The scan confirms the presence of significant left-sided proptosis. There is marked oedema of the left lateral rectus muscle but this does not appear to involve the tendinous insertion. There is similar, but less marked oedema of the left superior and inferior rectus muscles. The other extraocular muscles on the left and on the right are normal in appearance. The left lacrimal gland also appears oedematous. There is mild enhancement of the affected extraocular muscles and the left lacrimal gland following IV contrast. Normal appearances of both optic nerves. No evidence of significant intraconal or extraconal mass lesions on either side. The globes are unremarkable in appearance. There is a significant oedema in the skin and subcutaneous tissues around the left orbit.
As seen in Figure 1, MRI orbits confirmed the presence of a significant left-sided proptosis secondary to extraocular muscle and lacrimal gland enlargement. MRI head, MRI cerebral veins, and MRA head were noted to be normal.
It was assumed the small, tender pruritic patch on the upper eyelid, together with the fact that the patient had her window open overnight, was suggestive of an insect bite. Following senior ophthalmology review and largely normal blood test results (except for a mildly raised erythrocyte sedimentation rate, white cell count and neutrophil count), a diagnosis of orbital inflammatory syndrome (OIS), secondary to a suspected insect bite, was made. This likely resulted in a rapid compression of all structures, with subsequent compressive optic neuropathy and CRAO.
Despite prompt appropriate ophthalmic management and close outpatient monitoring, this patient sadly did not regain vision in her left eye and was referred onwards to the Eye Clinic Liaison Officer (ECLO) for additional support.
What is OIS?
Since the first description of OIS in 1905 by Birch-Hirschfeld under the name ‘orbital pseudotumour’, our understanding of this disorder has remained complicated by the wide spectrum of clinical and histologic presentations of the disease [1, 2]. OIS, also known as idiopathic orbital inflammation (IOI) and non-specific orbital inflammation (NSOI), is defined as “a benign, non-infective clinical syndrome characterised by features of non-specific inflammatory conditions of the orbit most often without an identifiable cause” [2]. The initial term ‘pseudotumour’ described an orbital neoplasm-like mass on presentation but which was found to be histologically inflammatory [2].
“A benign, non-infective clinical syndrome characterised by features of non-specific inflammatory conditions of the orbit most often without an identifiable cause”
OIS is the most common cause of painful orbital mass in adults and the third most common orbital disease after thyroid eye disease and orbital lymphoma; it affects all ages and accounts for approximately 6% of all orbital diseases [3,4,5]. Peak incidence is between the fourth and fifth decade of life, but children comprise around 17% of all OIS cases [2,6].
The aetiology and pathogenesis has not yet been identified, however, infectious and immune-mediated aetiologies have been implicated [3]. The process can primarily affect the lacrimal gland (dacryoadenitis), extraocular muscles (myositis), the sclera (scleritis), posterior tenons (tenonitis), intraocular uvea (uveitis), optic nerve sheath (optic neuritis), or the superior orbital fissure and cavernous sinus (Tolosa-Hunt syndrome), or the process may diffusely involve the orbital fatty tissues [1]. Histological findings can vary widely but are generally characterised by non-granulomatous inflammatory infiltrates, predominantly lymphocytic T-cells, which can be focal or diffuse [7].
OIS in adults is usually unilateral and the most common presentation is with sudden or sub-acute onset of pain (typified by a deep, boring orbital ache and headache) and peri-orbital swelling [1, 6]. Periorbital swelling is also the most common sign and occurs 75-79.2% of the time followed by proptosis (32-62.5%), extraocular muscle restriction (54.2%), red eye (48%), chemosis (29%), decreased visual acuity (20.8%), and ptosis (16.7%). Paediatric OIS differs from the adult presentation and is more commonly characterised by bilateral manifestation of uveitis, disc oedema and eosinophilia. Bilateral involvement is present in approximately 45% of paediatric patients versus 25% of adults [2, 4]. Furthermore, in paediatric cases, proptosis is usually mild or moderate, loss of visual acuity is common, and periorbital swelling tends to be worse in the morning with improvement throughout the day [2]. Approximately 50% of affected children also report systemic symptoms, including headache, vomiting, sore throat, or fever [2].
Differential diagnoses
There are eight sub-classifications of OIS depending on which structures in the orbit are affected by the infiltrates: anterior OIS, diffuse OIS, apical OIS, myositis, dacryoadenitis, peri-scleritis, perineuritis and focal mass. Each sub-classification comes with a host of differentials which need to be ruled out before a definitive diagnosis can be made [7].
The most common orbital processes that can present with the same clinical picture as OIS are orbital cellulitis and thyroid eye disease (TED) [1].
Management
OIS is a diagnosis of exclusion, and is made only after all other causes of inflammation have been eliminated [4]. A thorough history and physical examination are necessary for all patients with evidence of orbital inflammation - in particular searching for any signs of systemic illness such as infection, thyroid disease, autoimmune disease, or malignancy [2].
A full ophthalmic examination should be completed. This should include eyelid assessment (retraction/lid lag/lagophthalmos), orbital assessment (proptosis), extraocular muscles (restriction), globe (hyperaemia/chemosis), and optic nerve function (visual acuity/colour vision/relative afferent pupillary defect) [4].
Blood test:
The typical initial laboratory work-up should include a complete blood count, basic metabolic panel, thyroid function studies, erythrocyte sedimentation rate, antinuclear antibodies and antineutrophil cytoplasmic antibodies [4]. Examples of additional laboratory tests to consider include angiotensin-converting enzyme and rheumatoid factor [2]. The complete blood count, inflammatory markers and other results that test for the differential diagnoses as aforementioned are usually found to be within normal limits. However, mild elevation of the leukocyte count and erythrocyte sedimentation rate, as well as eosinophilia, may be seen [8].
Imaging:
Orbital imaging, through high-resolution computed tomography (CT) or contrast-enhanced magnetic resonance imaging (MRI), is appropriate for all patients suspected to have orbital inflammation, as characteristic imaging findings may help to distinguish between the differential diagnoses [2,4]. Imaging findings will be dependent on the structures involved and may identify enlargement of periorbital tissues: dacryoadenitis and myositis are common findings. Any bone involvement argues against IOS and suggests infection or malignant disease [2,8]. Orbital cellulitis, a common differential diagnosis, would be accompanied by evidence of underlying sinus infection on imaging in 75% of cases [2].
Biopsy:
The Mottow and Jakobiec study reported increased residua of disease in patients with OIS who underwent biopsy [8]. Therefore, biopsy is generally not performed as part of the initial evaluation but may be appropriate for atypical cases, those refractory to initial management, or in suspected malignant disease [2,8].
Corticosteroids are the mainstay of therapy and many patients improve with short courses. Rapid responses to corticosteroid therapy supports the diagnosis of OIS [2,8]. However, multiple other treatment options are available and include simple observation +/- NSAIDs for mild cases, radiation therapy for cases with insufficient response to corticosteroids or for whom corticosteroids are contraindicated, as well as chemotherapeutic agents and surgery [1,4].
Conclusion
Despite being the most common cause of painful orbital mass in adults and the third most common orbital disease, OIS still proves to be a difficult ocular condition to diagnose, treat, and manage. It is important to rule out other diagnoses before making a definitive diagnosis. It is also equally important to diagnose IOS in a timely manner because any orbital tissue could be affected, from compression on the optic nerve to exposure keratopathy [7]. Vision loss is the most devastating potential complication of this condition, as observed in our patient, and further highlights the urgent need for timely recognition and management [6]. Bringing attention to this topic will help to spread awareness amongst doctors, especially non-ophthalmologists who would otherwise have very minimal exposure to such presentations.
References
1. Espinoza GM. Orbital inflammatory pseudotumors: etiology, differential diagnosis, and management. Curr Rheumatol Rep 2010;12(6):443.
2. LaPonsie SA, Rabiah PK. When an orbital infection isn’t infectious at all: A review of orbital inflammatory syndrome. Pediatric Annals 2017;46(11):e443-6
3. Rabina G, Leibovitch I, Abumanhal M, et al. Orbital inflammatory syndrome post group a streptococcal infection - case series and review of literature. Ocul immunol and Inflamm 2019;27(1):162-7.
4. EyeWiki. American Academy of Ophthalmology.
https://eyewiki.aao.org/Nonspecific_Orbital_Inflammation_
(Idiopathic_Orbital_Inflammation,_Orbital_Inflammatory_Syndrome,_
Orbital_Pseudotumor)#Differential_Diagnosis
Last accessed October 2021.
5. Savino G, Battendieri R, Siniscalco A, et al. Intraorbital injection of Rituximab in idiopathic orbital inflammatory syndrome: case reports. Rheumatol Int 2015;35(1):183-8.
6. Idiopathic Orbital Inflammation – American Academy of Ophthalmology
https://www.aao.org/oculoplastics-center/
idiopathic-orbital-inflammation
Last accessed October 2021.
7. Warner B. Differential key to diagnosing idiopathic orbital inflammation. Optom Times 2021;13(2):24-6.
8. Chang TS, Sunkara SM, Cooley AS. Adolescent with right orbital swelling and proptosis. Idiopathic orbital inflammatory syndrome. JAMA Pediatr 2014;168(7):677-8.
COMMENTS ARE WELCOME







