A report from Monitor in October 2015 identifies good practices that will realise most of the potential productivity gain in elective care available to NHS hospitals. These include: stratifying patients by risk and creating low-complexity pathways for lower-risk patients (tailoring pathways to the risk profile of each group); extending clinical roles to enable lower-grade staff to undertake routine tasks in theatre or outpatient clinics usually performed by consultants; and providing virtual follow-up for uncomplicated patients (virtual clinics).
The author talks to medical retina specialists at five different treatment centres in England about current development initiatives in macular service provision, illustrating practice advances and an active commitment to excellence in ophthalmology.
Networked image management system at Kingston improves patient-based retina assessment in busy clinics
Vasuki Sivagnanavel, Lead Medical Retina Consultant, Kingston Hospital, London, said that a single networked image management system can improve service delivery in retina care, and simplify consultant-led oversight of community-based care initiatives for discharged patients.
“All hospital eye units are under strain to deliver an effective retina service for neovascular (wet) age-related macular degeneration (AMD), diabetic macular oedema (DMO) and retinal vein occlusion (RVO),” said Miss Sivagnanavel. “At Kingston Hospital, the retina clinic deals with approximately 250 new patient attendances each year, an incidence level that is higher than the national average. Capacity and resource constraints meant we needed to consider different ways of providing a fast-expanding retina service.”
Faster clinic throughput
As part of ongoing service improvements and to facilitate virtual or remote community-based monitoring, the Kingston eye unit recently introduced the clinic’s first fully networked image management system using Topcon’s Synergy Ophthalmic Data Management System. This is a web-based system that allows integrated patient-based outcome assessment, providing remote or onsite access to current and historical patient image scans obtained from multiple devices and locations.
“Having a single networked system to access all patient imaging data makes clinic throughput faster, and facilitates prompt decision making in a single visit,” Miss Sivagnanavel explained. “This avoids reduplication of clinic visits or delays due to inaccessible or unavailable imaging data. Accessing a single integrated system also improves patient safety, as all relevant diagnostic information can be made available at every visit, including remote sites that the hospital may serve in.
“The Synergy system may be used as a means to support more community care initiatives involving allied healthcare professionals for the monitoring and observation of stable patients who are subsequently discharged. This can free up space and capacity in the retina clinic, yet still ensures continuation of consultant-managed care with the use of the Synergy system for remote and rapid review of patient information.”
Releasing capacity using a treat and extend approach
“We operate a one-stop monitoring and intravitreal antivascular endothelial growth factor (anti-VEGF) injection service in our AMD clinic, and at present there is a two-stop service for DMO and RVO,” added Miss Sivagnanavel. “Optical coherence tomography (OCT) imaging assessment is carried out at each patient visit to determine treatment response and to monitor for fellow eye involvement.
“I believe the best way forward in the management of DMO and RVO is a treat and extend model based on visual and anatomic outcomes, as adopted in the wet AMD clinic. This approach can help minimise clinic visits and release capacity. A treat and extend regimen using intravitreal anti-VEGF therapy might also potentially reduce overall drug use by avoiding unnecessary retreatment.”
Emergency Macular Service in Manchester prioritises referrals for faster access to macular treatment
Sajjad Mahmood, Consultant Ophthalmic Surgeon and Lead Clinician for the Macular Treatment Centre at Manchester Royal Eye Hospital, explained how the unit has utilised the training of its specialist optometrists and OCT imaging technology in a newly-introduced Emergency Macular Service (EMAC). This service initiative provides a streamlined in-house triage approach to ensure accurate early diagnosis and prompter access to treatment for individuals with macular disorders.
“The Emergency Macular Service, set up in May 2015, provides a rapid access, virtual triage service for referred patients with suspect or confirmed macular problems,” said Mr Mahmood. “It ensures prioritisation and direct referral to the macular treatment centre for urgent treatment of patients with wet AMD, central RVO and myopic choroidal neovascularisation. Less urgent conditions such as branch RVO, DMO or macular hole are triaged for review in outpatient clinics with a medical or surgical retina consultant.
“High-street optometrists are able now to refer an individual direct to the EMAC service at Manchester Royal Eye Hospital if they have any concerns over potential macular issues, without the need for prior OCT imaging assessment or detailed completion of referral forms. We found in the past that despite best efforts, some individuals with macular disease were slipping through the net, going undetected and receiving delayed treatment.”
Prompt access to treatment to prevent further sight loss
“The Emergency Macular Service functions as a walk-in service, offering same day assessment if the patient can attend or at least aiming for an appointment within 48 hours from first contact. A nurse checks visual acuity and an ‘ophthalmic science practitioner’ carries out an OCT scan. Specialist trained optometrists review the OCT imaging quickly within 24 hours and decide on the best onward referral route for the patient. This helps to quickly identify cases that require urgent intravitreal treatment to prevent further sight loss (treatment aimed within two weeks from referral).”
Mr Mahmood added, “There is clearly demand in the community for this emergency assessment and triage service for individuals with suspected macular problems. The service effectively removes much of the anxiety over referral practice, such as false positive or inadequate referrals. We’ve received highly positive feedback from community optometrists. EMAC assesses and triages around 60 new patients each month. The main benefit is accurate macular assessment using OCT, and faster assess to treatment for those with confirmed sight-threatening macular conditions.”

Figure 1: EMAC service pathway. EMAC, Emergency Macular; AMD, age-related macular degeneration; CNV, choroidal neovascularisation; CRVO/BRVO, central/branch retinal vein occlusion; DMO, diabetic macular oedema; CSR, central serous retinopathy; VMT, vitreomacular traction; ERM, epiretinal membrane.
Figure 1 illustrates key steps in the triage process within the Emergency Macular Service at Manchester Royal Eye Hospital.
Sheffield data show potential of low-voltage x-ray irradiation for treatment naïve wet AMD patients
INTREPID is a sham-controlled masked study of external beam low-energy x-ray (16 Gray) stereotactic radiotherapy (Oraya Therapy, Oraya Inc) adjunctive to as-needed anti-VEGF injections for treating neovascular AMD. Trial data show that a single dose of stereotactic radiotherapy in chronic neovascular AMD patients previously treated with antiangiogenic therapy significantly reduces the number of necessary intravitreal anti-VEGF retreatments over two years [1]. The best response was seen in patients with smaller lesions (≤4mm greatest linear dimension (GLD), the size of the IRay® treatment zone) and with high macular volume (>7.4 mm3). Ophthalmologists in Germany and the UK recently confirmed results from early initial practice experience, indicating that Oraya Therapy is effective as a one-time procedure in maintaining or improving vision with a low anti-VEGF injection frequency in chronic wet AMD and newly-diagnosed wet AMD patients.
Royal Hallamshire Hospital (RHH) in Sheffield was the first NHS centre in the UK to offer Oraya Therapy to suitable newly-diagnosed wet AMD patients, commencing in May 2014. Eligible patients must have an active lesion, with a GLD less than 4mm on fluorescein angiography centred on the fovea, minimal fibrosis, abnormal macular thickness and an axial length between 20-26mm. Stereotactic radiotherapy is given within two weeks of the first anti-VEGF injection.
Presented for the first time at the EURETINA 15 Congress in Nice, France, one-year outcomes in a small case series of 25 treatment-naive wet AMD patients treated with Oraya Therapy at RHH show a mean change in best corrected visual acuity (BCVA) from baseline of +5.0 Early Treatment of Diabetic Retinopathy Study (ETDRS) letters, and a mean of 4.6 anti-VEGF injections given during the year. One third of these patients required only three anti-VEGF injections given as part of the recommended treatment loading phase. For a comparator ‘control’ group of 41 consecutive patients diagnosed with neovascular AMD immediately prior to the introduction of Oraya Therapy and who met the Oraya treatment criteria, the mean VA change from baseline to month 12 was -0.3 letters on as-needed ranibizumab (Lucentis, Novartis) monotherapy, and with a mean of 5.63 ranibizumab injections given.
In another Oraya-treated cohort involving the first 58 wet AMD patients with six months’ follow-up since receiving their first ranibizumab injection, mean BCVA change from baseline to month six was just under four letters. In this series, 57% achieved VA 6/12 or better at six months compared with 41% at baseline. More than half (57%) required only the loading phase of three consecutive monthly ranibizumab injections.

Figure 2: Visual results in treatment naïve wet AMD patients, as needed ranibizumab with and without (comparator) adjunctive stereotactic radiotherapy (change in VA, letters). Source: Courtesy of Mr Christopher Brand, Royal Hallamshire Hospital, Sheffield, UK.
Figure 2 shows visual outcomes for all three treatment cohorts, Figure 3 details retreatment episodes through 12 months for the Oraya-treated series and Sheffield comparator group.
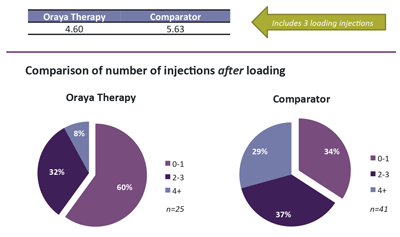
Figure 3: Anti-VEGF injections at 12 months after diagnosis and treatment start, as needed ranibizumab with and without (comparator) adjunctive stereotactic radiotherapy. Source: Courtesy of Mr Christopher Brand, Royal Hallamshire Hospital, Sheffield, UK.
Christopher Brand, Consultant Ophthalmologist, Royal Hallamshire Hospital, commented: “Clinical outcomes show that treatment with stereotactic radiotherapy administered during the anti-VEGF loading phase for treatment naïve wet AMD patients reduces the number of necessary anti-VEGF retreatments over the course of one year, with excellent visual outcomes achieved in vision stabilisation and / or VA improvement from baseline, compared with standard of care anti-VEGF monotherapy as required. Adjunctive treatment with Oraya Therapy was well tolerated, with no evidence of retinal microvascular abnormalities or excessive fibrotic proliferation.”
Award-winning macular service at Good Hope Hospital
“Guidelines, modern management policies, training of optometry and medical staff, flexibility, modern information technology, teamwork, and effective leadership are key components in delivering an efficient macular service,” explained Ramesh Sivaraj, Consultant Ophthalmologist and Clinical Director of Ophthalmology, Good Hope Hospital (GHH), Birmingham.
The macular service at Good Hope Hospital forms part of a district general hospital, and is one of three centres of the Heart of England NHS Foundation Trust (HEFT) Ophthalmology directorate. Staff provide cross cover, unit equipment is linked to a server-based imaging database, and an electronic patient record system provides a good governance and audit tool.
Referrals
More than 50% of patients are referred through GHH rapid access macular service (RAM) using a fast track referral form, and other patients may be referred from other clinics. Additional referral routes include tertiary grading at diabetic screening, which is undertaken by a consultant working in the unit, and transfer of care from nearby units. “We have noted that patients present earlier due to improved awareness and optometrist education,” commented Mr Sivaraj. “This has resulted in better prognosis. We also provide regular feedback letters to GPs and optometrists, which helps to improve quality of referrals. We are piloting an electronic telemedicine referral service through a nhs.net email contact, which provides additional advice and guidance.”

Figure 4: Anti-VEGF in wet AMD pathway.

Figure 5: Oraya in wet AMD pathway.
Treatment
Newly-diagnosed wet AMD patients are offered anti-VEGF treatment with aflibercept (Eylea, Bayer) or ranibizumab, and adjunctive stereotactic radiotherapy for eligible eyes (Figure 4 and 5 show respective pathways). Treatment and care protocols are developed in collaboration with all ophthalmology personnel and revised or updated as necessary every six months. Injections are provided by all members of the medial retina team including a trained nurse injector. Two additional nurses are undergoing training for administration of intravitreal injections. Where possible, the first intravitreal anti-VEGF injection is given in the afternoon following the morning RAM clinic but otherwise within the next few days.
Mr Sivaraj commented, “The aim is to inject as soon as possible following diagnosis. Our unit has also treated over 100 eyes with Oraya Therapy and now have six month follow-up for 35 patients, which we are analysing. There are several research studies conducted at all three sites, including the provision of a treatment centre for the 24-month Stereotactic Radiotherapy for Wet AMD (STAR) trial.”
Reviews
Reviews are undertaken in virtual macular clinics (VMC) where the patient meets the nurse who records if there has been any change in health status and discusses visual function in the treated and fellow eye. The logMAR vision is checked and the patient is dilated for OCT imaging scan. The technicians who run this clinic are trained to make treatment decisions and often discuss treatment with the patient. A doctor is available to discuss if needed. The patient usually spends 30-40 minutes in the hospital, with an appointment schedule then confirmed by the unit coordinator.
“Patients who have been stable have an option of follow-up with a high street optician who can relay scans and other details direct to us through hospital net,” Mr Sivaraj added. “We will shortly be able to view OCT video through the existing N3 NHS broadband with adjustments to firewalls (pilot project), aiming for virtual service provision across the region when the pilot has completed. The low vision service is run by two experienced part-time optometrists, with sight impairment certification completed if necessary.”
Mr Sivaraj and his team at Good Hope Hospital won a 2015 Clinical Service of the Year award in the annual recognition of excellence from the Macular Society.
Frimley Park Hospital extends clinical roles, effective measures that increase treatment capacity
Frimley Park Hospital in Surrey has introduced both an orthoptist-delivered and an ophthalmic specialist nurse-delivered intravitreal injection service. Appropriate indemnity and standard operating procedures were implemented before commencement of any training, and regular ongoing audits and competency reviews are conducted to ensure patient safety. The orthoptic consultant and ophthalmic specialist nurses commenced their intravitreal injection training at the same time, and each performed 100 intravitreal injections under direct supervision by a doctor prior to approval of independent practice. “Audit results show no serious or sight-threatening complications, with little variation in patient experience when compared to a doctor-led injection service [2,3],” commented Professor Geeta Menon, Consultant Ophthalmic Surgeon, Frimley Health NHS Foundation Trust. “Both initiatives have significantly increased medical retina treatment capacity.”
A study by Da Costa et al. evaluated patient safety, patient experience, and clinic capacity following the implementation of a nurse-delivered intravitreal injection service at Moorfields Eye Hospital, London [4]. Results show no serious vision-threatening complications in a consecutive series of 4,000 nurse-delivered intravitreal injections over a 24-month period. There was a significant increase in intravitreal injection capacity in medical retina clinics following implementation of the nurse injector initiative. Utilising trained nurses to deliver injectable treatments of ranibizumab and aflibercept for neovascular AMD allows the retina service to become an effective one-stop service where treatment is administered on the same day the diagnosis / treatment decision is made. Enablers include a formalised training programme for specialist nurses, supporting protocols, governance and supervision, as well as supporting legal framework to address drug licensing requirements and litigation risk.
References
1. Jackson TL, Chakravarthy U, Slakter JS; INTREPID Study Group. Stereotactic radiotherapy for neovascular age-related macular degeneration: year 2 results of the INTREPID study. Ophthalmology 2015;122:138-45.
2. North L, Chandran M, Menon G. Orthoptist-delivered intravitreal anti-VEGF injections. Royal College of Ophthalmologists annual congress 2015;19-21 May 2015, poster presentation.
3. Raguro A, Bisain L, Gencheva P, et al. Implementation of a nurse-delivered intravitreal injection service. ARVO 2015 annual meeting; 3-7 May 2015, poster presentation.
4. DaCosta J, Hamilton R, Nago J, et al. Implementation of a nurse-delivered intravitreal injection service. Eye (Lond) 2014;28:734-40.
TAKE HOME MESSAGE
-
Good practices for delivering productivity gains in ophthalmology practice include:
-
Stratify patients by risk and tailor pathways to the risk profile of each group.
-
Extend clinical roles to enable lower-grade staff to undertake routine tasks in theatre or outpatient clinics usually performed by consultants.
-
Use technology to help provide virtual follow-up for uncomplicated or stable patients.
COMMENTS ARE WELCOME





