
The COVID-19 Urgent Eyecare Services (CUES) was developed to relieve the demands of hospital ophthalmology, aiming to allow patients to have remote consultations and be managed by community optometric practice. This was because access to Hospital Eye Service (HES) Ophthalmic Casualty was reduced as HES clinicians were redeployed. The aim of this study was to evaluate those CUES patients, seen solely by primary care optometrists, who might previously have been managed in secondary care, and if independent prescribing (IP) facilitated this.
Introduction
The manifestation of the COVID-19 pandemic due to SARS-CoV-2 coronavirus instigated uncertainty in optometric practice, with the initial cessation of routine sight tests and the introduction of personal protective equipment (PPE). The College of Optometrists, the Royal College of Ophthalmologists, and the National Health Service (NHS) England / Improvement worked together to establish CUES. Whilst this could be commissioned by any clinical commissioning group (CCG), many chose to contract this to Primary Eyecare Services (PES) [1].
CUES was developed to allow urgent and emergency eyecare to be commissioned through contracts with local commissioners (Integrated Care Systems / Sustainability and Transformation Partnerships, and CCGs) [1]. This was a consequence of the cessation of routine sight testing during the first lockdown, commencing on 23 March 2020 in the UK [1]. Objectives of CUES included safe delivery of community eyecare whilst reducing face-to-face interactions with remote triage and consultations [1]. Furthermore, reducing the burden on general practitioners (GPs) and HES in secondary care allowed hospital workforce redeployment for front-line COVID-19 response efforts [1]. It was crucial, considering the pandemic, to implement services in locations where enhanced clinical pathways did not already exist to ensure no areas were disadvantaged [2]. Some existing pathways, including the Minor Eye Conditions Service (MECS), independent of CUES, were designed to achieve similar objectives e.g., avoiding unnecessary referrals by managing acute conditions within community practice [3]. The CUES patient pathway (Figure 1) was developed and implemented in three weeks. This pathway highlights the significance of initial remote telephone consultations, before discharging with self-care advice, having a face-to-face consultation in practice or onwards referral to GP / HES.
MECS in Herefordshire did not originally include remote consultations, or permit access to FP10 NHS prescribing for IP-qualified optometrists – previously, patients were seen in person before optometrists decided to self-manage, if necessary with a private medicines prescription, or refered to HES [4]. Herefordshire CCG worked closely with Herefordshire Local Optical Committee (LOC) and the Wye Valley NHS Trust Hospital and, within 48 hours of plans to lockdown nationally and the emergence of the Trust resilience plan, were able to commission a remote access funding model of the existing MECS scheme. Similarly, the previously unobtainable FP10 NHS prescription pads were made available to all IP optometrists. Initially these were HES pads (funded from HES budget) but latterly (July 2020) switched to community funding. In Herefordshire, CUES replaced MECS on 1 July 2020 and is still in operation although the contract is held with PES, not directly with the CCG as MECS had been.
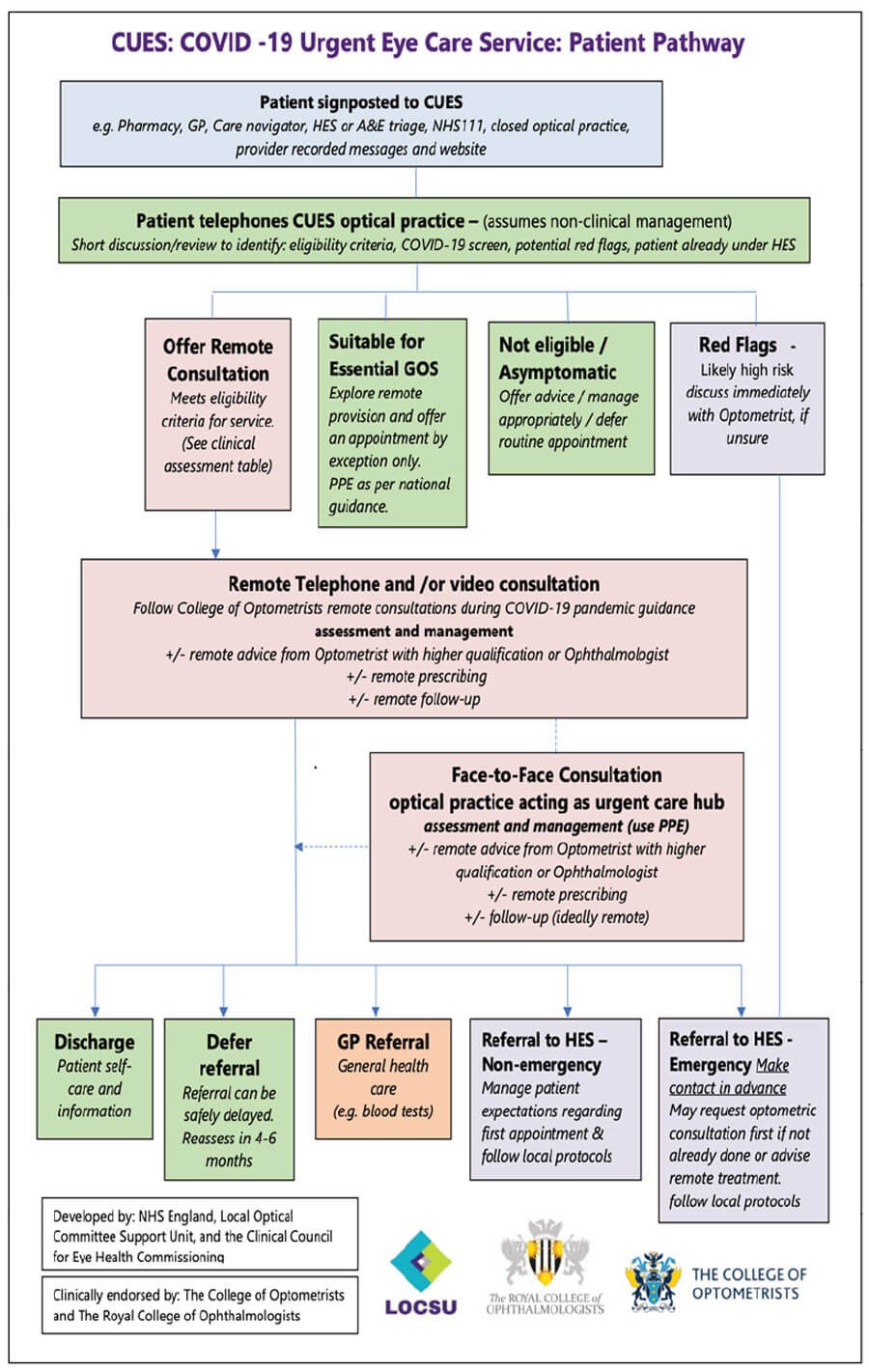
Figure 1: Showing a flow chart of the CUES patient pathway [1].
The aim of this study was to evaluate the null hypothesis that the introduction of CUES meant that patients seen in primary care would also be referred into secondary care, thus achieving no net reduction. Although primary care, in the context of NHS provision, is usually defined as including GPs, in this study GPs will be included as secondary care with HES on the basis that onward referrals to GPs were required when patients couldn’t be fully managed in practice. This study focuses on how many patients were referred to HES/GPs after the introduction of CUES, and thus if the objectives of CUES were met. This study also explores if IP optometrists played a role in reducing the number of referrals. IP is a post-graduate qualification allowing optometrists to prescribe any drug (oral and topical) from the British National Formulary for conditions affecting the eye and adnexa, with a few exceptions, providing it is within the practitioner’s scope of expertise [5]. Non-IP optometrists are only able to use and occasionally supply a short list of diagnostic and therapeutic Prescription Only Medicines (POMs) [6], however in Herefordshire, only IP-optometrists had access to FP10 pads. Therapeutics prescribed at BBR Optometry by IP optometrists within CUES are listed (Table 1).
The CUES patient pathway (Figure 1) highlights the ability of optometrists, with higher qualifications such as IP, to offer advice and prescribe treatments before referring to the GP / HES.
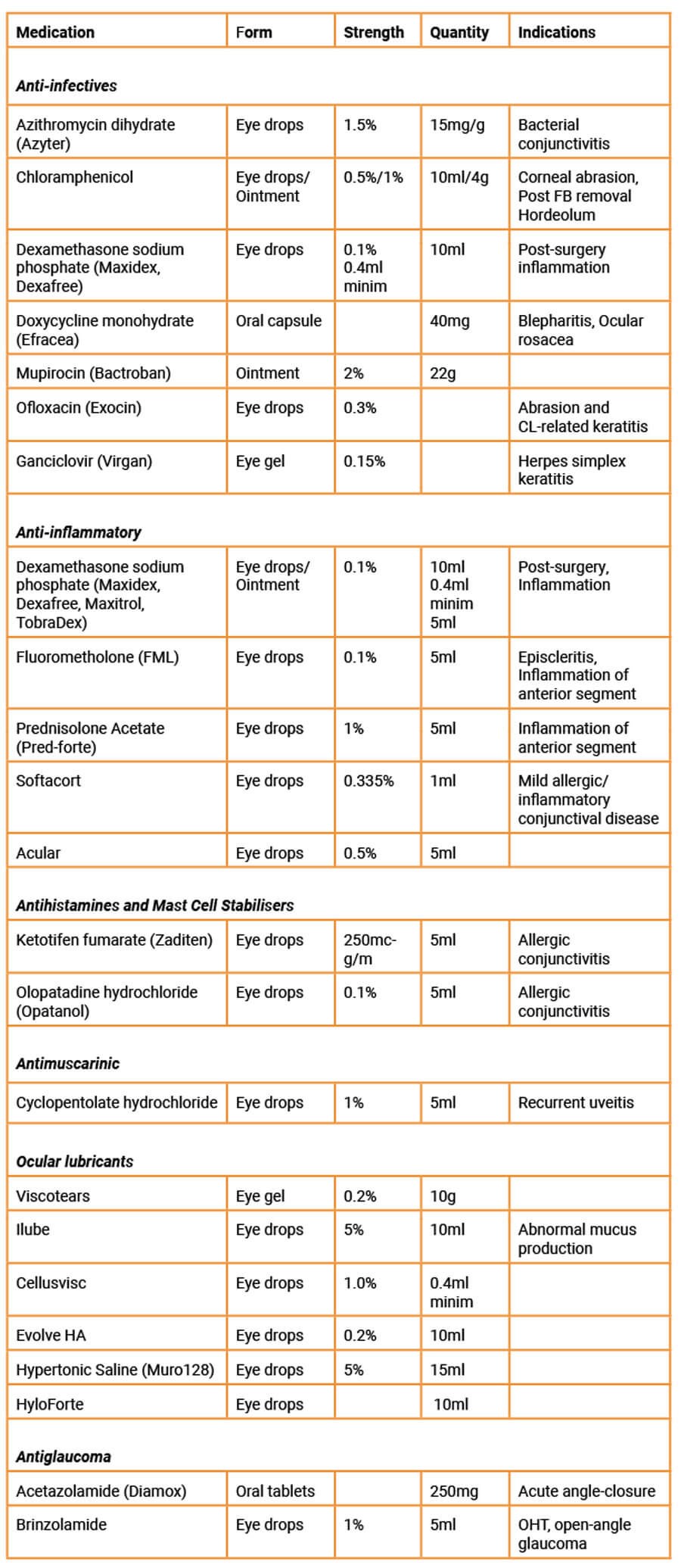 Table 1: The ocular therapeutics used at BBR Optometry by IP-optometrists,
Table 1: The ocular therapeutics used at BBR Optometry by IP-optometrists,
including some indications, to be prescribed via FP10s.
A secondary aim was to decipher if changes in UK government COVID-19 guidance affected the number of patients seen in person. Data was collected and allotted into five time periods across the course of the pandemic (Table 2), signifying the stages of the pandemic. This allows easier comparison of patients managed via telephone consultation or in person throughout different stages of the pandemic.
Method
This study collated data from 23 March 2020 to 31 December 2020, deciphering how many CUES patients at BBR Optometry were managed in practice (with or without the aid of IP optometrists) or were referred to GP / HES. It also indicates any relationships between changes in UK COVID-19 guidelines and the number of referrals to GPs/HES, by comparing data in five significant periods of the pandemic. From 23 March, routine sight tests were suspended with practices urged to offer only essential services based on clinical needs and urgent eye care pathways [8]. Final CUES guidance and specification was released 17 April 2020 [1].
Data was collected from BBR Optometry, the only independent optometric practice within Hereford, UK. At the time of data collection, three of five resident optometrists at BBR Optometry were IP-qualified. All patients received telemedicine appointments, with / without face-to-face appointments and onward referrals to the Victoria Eye Unit (VEU), Hereford. This data was recorded for all patients since 23 March 2020.
During period 1, the UK government enforced the first lockdown at the first peak of the pandemic. Routine sight tests were suspended [8] and BBR Optometry offered adapted MECS services for only urgent and emergency clinical presentations before the introduction of CUES. On 10 May 2020, the government released plans for the easing of lockdown [9]. Three optometrists, two of which were IP-qualified, collected data on an Excel spreadsheet, recording information from patient interactions: diagnosis, management (including IP), and referrals to GP / HES. Additionally, these patient interactions were input into PharmOutcomes, a secure clinical service platform for community commissioners to gather outcomes data for local services under direct contract with Herefordshire CCG. Data from both the Excel spreadsheet and PharmOutcomes were compared and combined as there was some discrepancies with patients missing from the spreadsheet. This ensured no patient data was missed. There was also a risk of double counting, therefore patients seen on the same day with the same details, including condition and management, were assumed to be the same patient.
From 1 June 2020, the government allowed gradual easing of lockdown restrictions; some children returned to schools, and by 15 June 2020, England’s retail parks, high streets, and shopping centres reopened [9]. Most data from period 2 was collected via PharmOutcomes, which logged patient presenting complaints, diagnoses, management (including IP), and referrals. In July 2020, Herefordshire CCG combined with Worcestershire CCG and commissioned PES to provide CUES. PES administers CUES through the proprietary OPERA platform. BBR Optometry therefore implemented the existing OPERA (Optometric Electronic Referral and Assessment) system on 1 July 2020 to better manage and record patient outcome data. Data from OPERA was used from 1 July onwards, therefore data from the last three days of period 2 was from OPERA alone. OPERA brings NHS IT infrastructure to primary optometric practice, facilitating easier collaboration between community practices [10], such as BBR Optometry, and GPs or HES such as the Victoria Eye Unit, Hereford. OPERA allows upgraded communication between optometrists, ophthalmologists, and GPs via access to non-degraded images, referral management, and asynchronous remote support [10,11].
Throughout period 3, pubs and restaurants reopened from 4 July 2020 [9]. However, by 30 July 2020, the UK government imposed local lockdowns in some parts of England [9]. By the end of August, a second national lockdown was being planned [9]. Data from here onwards was collected solely from OPERA, detailing diagnoses, management (including IP), and referrals to GP / HES.
Period 4 dates from 1 September to 4 November 2020. This period was important for CUES due to the growing fears of a second wave of COVID-19 [9]. Tighter restrictions were imposed during September 2020, including 10pm curfews for pubs / restaurants and a new 4-tier system for stricter local restrictions [9]. Meanwhile, Hereford remained in tier 2, with the least restrictions. By 31 October 2020, the UK had announced another four-week national lockdown [9].
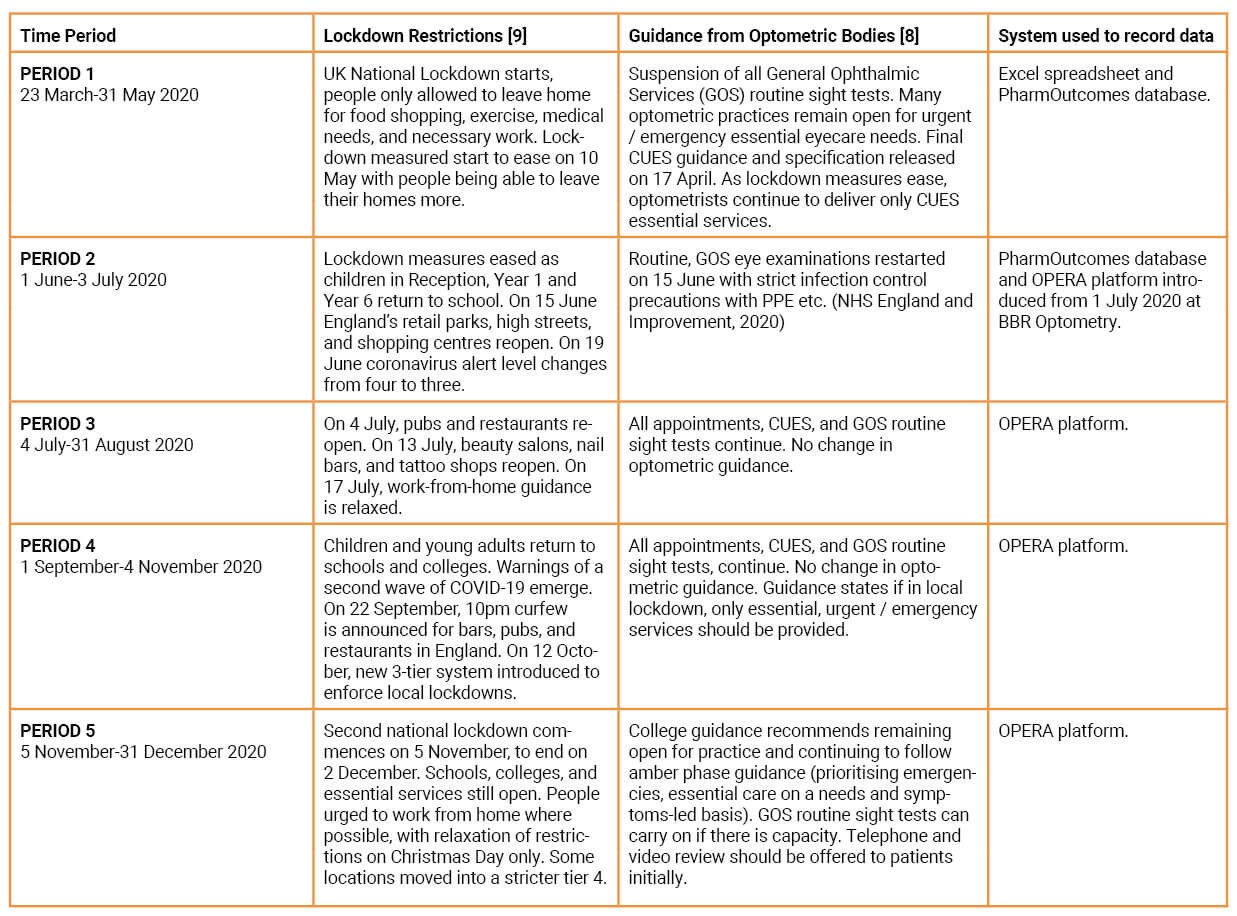
Table 2: The five time periods from 23 March 2020 to 31 December 2020.
Period 5 includes data from 5 November 2020 to 31 December 2020. The second national lockdown began and restrictions tightened with the closure of non-essential services [9]. After routine sight tests resumed on 15 July 2020, the College of Optometrists’ guidance remained for routine sight tests to continue, although it was advised to offer remote consultations initially [8]. The second national lockdown ended on 2 December 2020. A strict, 3-tier system remained, with a 4th tier added on 19 December 2020 in some areas [9]. Hereford remained in tiers 1 and 2 throughout this.
The management of patients was split into three groups:
Group 1 – Patients that could be managed by non-IP optometrists and did not have to be referred to secondary care (GP / HES). Patients were not prescribed any pharmacological treatments that were beyond the scope of non-IP optometrists. Includes patients being treated by chloramphenicol (eye drops 0.5% or ointment 1%) for superficial ocular infections, e.g. bacterial conjunctivitis, or prophylactically following minor ocular trauma [12] (see Table 2). Includes patients that were given remote advice as per CUES guidance (Figure 1).
Group 2 – Patients that could not be managed by non-IP optometrists, but were managed by IP-optometrists, avoiding referral to secondary care. The difficulty with putting some patients in group 2 is the argument that patients could be managed by non-IP optometrists, especially if therapeutics were prophylactic, e.g. a hordeolum treated with hot compresses and lid hygiene to self-resolve in group 1, or prescribed azithromycin dihydrate in group 2. Grouping of patients was therefore determined by the action taken, rather than possible management plans, regardless of whether therapeutics were prophylactic.
Group 3 – Patients that could not be managed in primary care by non-IP or IP-optometrists, therefore were referred to the GP or HES.
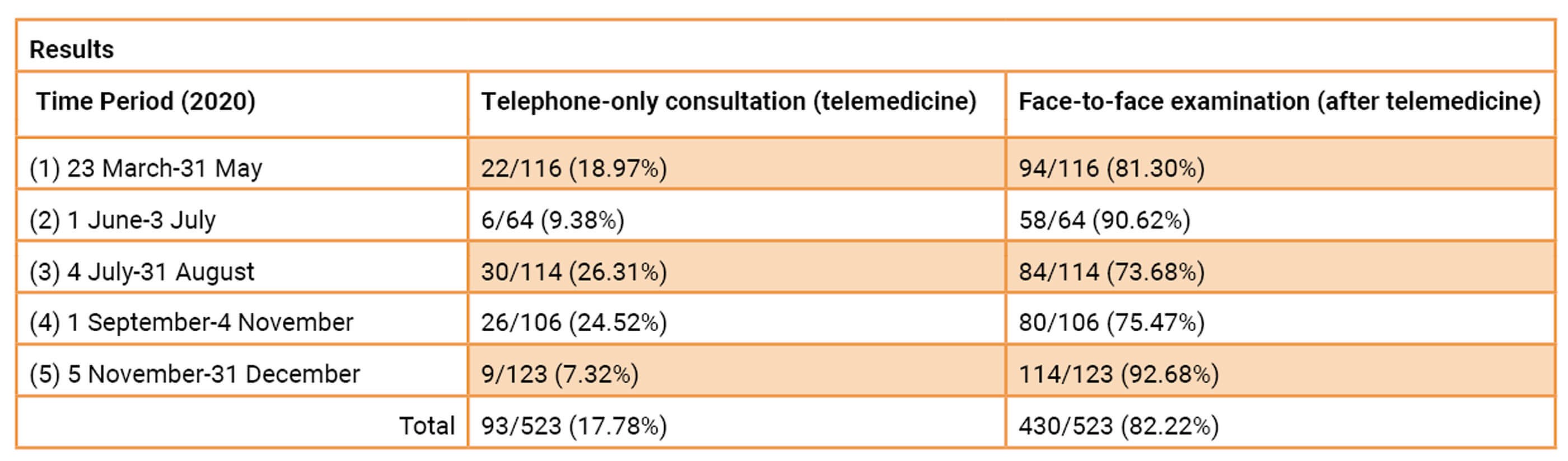 Table 3: The number of patients that were managed remotely via telephone consultation,
Table 3: The number of patients that were managed remotely via telephone consultation,
and those that required a further face-to-face examination in practice at BBR Optometry.
Table 3 details whether patients were managed by telephone consultation alone, or if they required face-to-face assessment. Throughout period 1, BBR Optometry recorded 116 patient interactions, 18.97% of which were managed remotely via telemedicine calls, and the remaining 81.30% had examinations in practice (with or without follow-up assessments). Some telemedicine calls included access to images taken by patients and occasionally video. This shows almost 1 in 5 patients were managed remotely, without having to expose themselves to others and increase their risk of contracting COVID-19. This was crucial initially in the pandemic when PPE was not readily available to optometric practice and optometrists worked to establish socially distanced routines.
During period 2, routine eye examinations resumed with strict infection control precautions in practice, such as PPE [3]. Data collected shows a rise (to 90.62%) of patients being seen in person within period 2 suggesting that as lockdown restrictions eased, more patients could be seen in practice.
Despite relaxation of lockdown restrictions [9] in period 3, numbers of patients managed remotely rose to 26.31%, the highest in this dataset, leading to fewer patients seen face-to-face (73.68%). There was little change during period 4, when concerns of a second wave arose and a new 3-tier system was introduced [9]. Period 4 exhibited around 1 in 4 patients (24.52%) being managed remotely and 75.47% qualifying for in-practice consultations.
The second national lockdown commenced in period 5, on 5 November 2020 [9]. Nevertheless, the proportion of patients managed remotely fell significantly to 7.32%, the lowest among all periods, with 93.68% requiring a face-to-face examination. Evidence shows many patients did not need to be seen in person at all, as 93 of 523 total patients (17.78%) were successfully managed remotely at BBR Optometry.
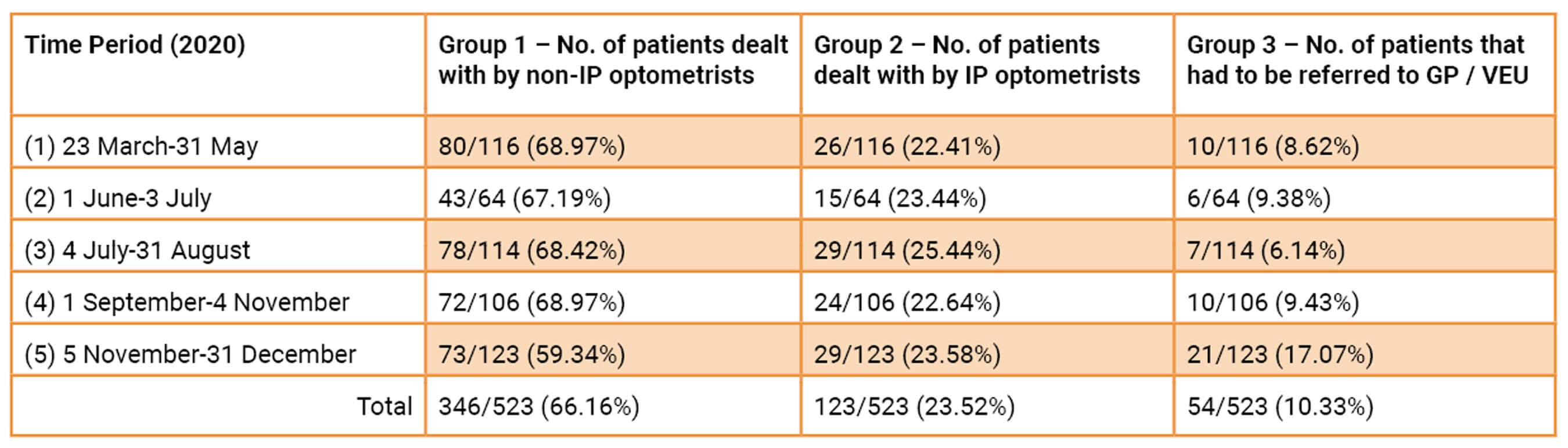
Table 4: The number of patients that could be managed by IP optometrists, non-IP optometrists,
and those that had to be referred into secondary care in different periods of the COVID-19 pandemic.
Table 4 displays how many patients in each period presented at BBR Optometry and in which group (1, 2 or 3) they were placed. Many CUES patients were managed solely in primary care, with only 54/523 (10.33%) patients referred to GP/VEU between 23 March and 31 December 2020. In addition, 346/523 (66.16%) could be managed by non-IP optometrists, and 123/523 (23.52%) were managed by IP-optometrists. Meaning, 469/523 (89.67%) of all CUES patients were managed in practice. One patient in this study was unsuccessfully treated by IP-optometrists, so required an onward referral, and was therefore placed into group 3.
Results show in period 1, 106/116 (91.37%) patients seen at BBR Optometry were managed in practice, with only 10/116 (8.62%) being referred to secondary care. Of these 106 patients, 26 were managed by IP optometrists, whom would have otherwise been referred to secondary care.
Throughout period 2, 64 CUES patients were seen at BBR optometry and 9.38% had to be referred to the VEU / GP. Of these 64 patients, the majority (67.19%) were able to be managed by non-IP optometrists, and 23.44% by IP optometrists. This was the shortest period with the least patients.
During period 3, the fewest patients (6.14%) from the 114 patients seen were referred to the VEU / GP. Of the remaining patients, 29/114 (25.44%) were managed by IP optometrists in practice, and 78/114 (68.42%) were able to be managed by non-IP optometrists. In period 4, referrals to the VEU / GP increased again to 9.43% of patients. Again, most patients could have been managed by non-IP optometrists (72/106, 68.97%), but 24/106 (22.64%) of patients were managed by IP optometrists.
Period 5 had the most CUES patients and number of onwards referrals to the VEU / GP (21/123, 17.07%), meaning fewer patients were managed in community. Of the 123 patients seen in period 5, 73 patients (59.34%) were managed by non-IP optometrists and 29 patients (23.58%) were managed by IP optometrists.
Discussion
A total of 523 patients undertook a CUES assessment at BBR Optometry during data collection. As noticed with the discrepancies between patients input into the PharmOutcomes system and BBR’s Microsoft Excel accounts in period 1, there may have been human error inputting patients into the OPERA system. Any patients unable to be seen within 24 hours, and thus referred to other CUES practices, were eliminated from this study.
The results indicate that CUES allowed many patients to be managed in primary care who would have otherwise been seen in secondary care / GP settings. 469/523 CUES patients seen at BBR Optometry were managed in practice, avoiding onwards referral. Without CCG’s commissioning practices to see these emergency patients, most of them would present in secondary care, especially during initial periods of the national lockdown. Additionally, there would be patients that would not attend any healthcare setting (GP / HES) in fear of contracting COVID-19 or the thought that their condition was not severe enough for secondary care. This means CUES has achieved its goal to alleviate pressures on GPs and ophthalmology departments within secondary care [1]. Moreover, it maintains local access to quality eyecare services for local populations [1].
In this study, 123 of 429 (28.67%) patients managed in practice were managed by IP optometrists. Patients were placed in group 2 by deciphering prescription of IP-only therapeutics, as highlighted in Figure 2. This is a significant number of patients who, otherwise, would be referred to HES / GP, emphasising the advantage of IP in community. CUES allows optometrists to better utilise their skills within community, which may have only been exercised for some roles in HES. Some patients, with the same diagnosis, were managed in different ways by both IP and non-IP optometrists, e.g. a hordeolum could be left to self-resolve by a non-IP optometrist but prescribed a mild corticosteroid to aid resolution. Some patients were treated by IP optometrists prophylactically, so they arguably could still have been managed conservatively by non-IP optometrists. This highlights that certain conditions are managed in different ways, depending on practitioner confidence, qualifications, and experience. One patient in this study, unsuccessfully treated by an IP optometrist, required an onward referral. This shows minimal duplication and hence wastage of NHS CCG resources. Despite the additional bureaucracy of NHS prescribing in IP, it is potentially the key to developing CUES in the future.
Currently IP optometrists are unevenly distributed, with many working in HES. The UK offers five IP courses, followed by hospital placements under the supervision of ophthalmologists to demonstrate clinical competency, and a final examination. There are now more than 620 optometrists qualified in IP, which represents approximately 5% of the 14,500 optometrists in practice [17]. The limiting factor for IP accreditation is the lack of hospital placements available – 12 days minimum of practical training is required under supervision of a consultant ophthalmologist [4]. With growing demand for optometrists to take further professional responsibility [5], especially due to the pandemic, this may be something governing bodies and CCGs could commission for long-term gain. The General Optical Council recognises this barrier and now permits up to 55% of clinical sessions for IP training to be completed remotely [5]. As more optometrists become IP qualified, they may, in the future, be able to train other optometrists for qualification. Research from Todd et al [13] supports community IP optometrists in their accurate diagnosis and management of acute conditions, being largely in concordance with ophthalmologists.
This analysis revealed conducting telephone consultations before face-to-face appointments allowed 93/523 (17.78%) patients to be managed remotely. Moreover, optometrists established a thorough history of symptoms remotely, allowing triaging in advance and less time with patients in practice. Reducing physical interactions was a key aim for CUES for the safety of patients and practitioners, and to allow more appointments for emergencies [1]. Interestingly, the highest percentage of face-to-face examinations was in period 5, when the second national lockdown commenced. This could be by chance, with more patients presenting with concerns requiring further investigation. It could also be due to Hereford remaining in tier 1 of the three-tier system, with minimal restrictions in part of November 2020, before being moved to tier 2. This could influence clinical decisions of BBR optometrists to see patients in person, if they felt the relative risk of transmitting COVID-19 was reduced. It would be expected that fewer patients would be seen face-to-face in period 1, at the height of the pandemic, when risk of COVID-19 transmission was higher. This is not the case, as 81.30% of patients required a physical examination. There could have been a greater difference in the number of patients seen in person between periods if data from a more at-risk area of the UK was analysed.
There is evidence of reduced HES [3] attendees after the introduction of CUES and several factors contribute to this. Firstly, CUES allows HES to reroute some patients back into community practice once remotely triaged, if ophthalmologists believe they can be managed in primary care. Secondly, it is possible that people are less likely to present in the community or HES / GP at all, especially with mild symptoms, if they are shielding from COVID-19 and are high-risk. For the same reason, it is possible fewer asymptomatic clinical emergencies are being detected, with fewer patients attending routine eye examinations (in fear of contracting COVID-19 or when routine examinations ceased). This could lead to a decline in reports of serious eye conditions, as well as fewer patients attending HES, giving a false narrative of the success of CUES in reducing those seen in secondary care.
Currently data is limited on the outcomes of CUES. Harper at el discuss the development and implementation of CUES in Greater Manchester [10]; more recently, Kanabar et el evaluated the outcomes of CUES in Manchester [15]. It was found that emergency eye department (EED) attendances were reduced by 37.7% per month between April and December 2020 with CUES, compared to the same months in 2019 [15]. They concluded the case-mix of patients presenting following referral to HES appeared to be of a less benign nature than those prior to CUES; most commonly, uveitis, age-related macular degeneration, and retinal vein occlusions, suggesting simpler cases were managed in community with CUES. Siempis found conjunctivitis and dry eye to be some of the most common acute eye conditions, and with self-referrals constituting most of the inflow to HES, CUES allows ophthalmologists to signpost patients to the community [15,16]. This is important as it highlights a large proportion of patients initially attending HES could be adequately managed in community practice, and even more so with IP optometrists. Kanabar et al highlights that several accepted referrals to EED could have been appropriately managed in the community by IP optometrists [15]. The study in this article supports this by providing useful analysis on the role of IP in reducing referrals to HES, with 23.52% (123/523) of patients in group 2. Referral rates with CUES found by Kanabar et al (14.3%) were lower than that found by Konstantakopoulou et al for MECS (19.3%) [15,3]. This could be because the MECS specification does not include remote consultations, despite many of its aims being consistent with CUES [4].
The COVID-19 pandemic propelled the development of a service to enhance practitioner-to-practitioner communication. This, undoubtedly, was lacking within optometric practice. Refining systems, such as OPERA, gives scope for better relationships between optometrists and ophthalmologists which would also be beneficial post-pandemic. The effectiveness of CUES still needs to be evaluated in more detail – the OPERA system could help analyse other aspects of CUES, such as the type of pathology presenting in community practice or where patients were referred from (self-referral or signposted from HES / GP).
In conclusion, this study contributes a clearer understanding of the positive impact of CUES to managing acute eye conditions in community practice. The importance of IP in the evolution of optometry is clear, especially as the NHS recovers from the aftermath of COVID-19. CUES steers patients away from secondary care and increases the responsibilities of community optometrists. Further development of CUES is required to enhance communication between primary and secondary care, and to train and deploy more IP optometrists into the community. As CUES is refined over the coming years, it may warrant a change in name, perhaps to Urgent Eye Care Service, as the COVID-19 pandemic resolves and a more permanent enhanced service is established.
References
1. COVID-19 Urgent Eyecare Service (CUES) in England. The College of Optometrists.
https://www.college-optometrists.org/
the-college/media-hub/news-listing/nhs-england
-covid-19-urgent-eyecare-service-cues.html
2. COVID-19 Urgent Eyecare Service (CUES). LOCSU.
https://www.locsu.co.uk/covid-19
-urgent-eyecare-service-cues/
3. Konstantakopoulou E, Edgar DF, Harper RA, et al. Evaluation of a minor eye conditions scheme delivered by community optometrists. BMJ open 2016;6(8).
4. Minor eye conditions service (MECS) pathway & protocols. Primary Eyecare Services.
https://hampshireloc.org.uk/wp-content/uploads/
2020/01/MECS-Pathway-Protocol-West
-Hampshire-Southampton-v3.pdf
5. Rumney N. Optometry and independent prescribing. Journal of Prescribing Practice 2019;1(2):87-92.
6. Needle JJ, Petchey R, Lawrenson JG. A survey of the scope of therapeutic practice by UK optometrists and their attitudes to an extended prescribing role. Ophthalmic and Physiological Optics 2008;28(3):193-203.
7. Prescription forms. NHS Business Services Authority.
https://www.nhsbsa.nhs.uk/pharmacies-gp
-practices-and-appliance-contractors/prescribing
-and-dispensing/prescription-forms
8. COVID-19: Member update archive. The College of Optometrists.
https://www.college-optometrists.org/
guidance/covid-19-coronavirus-guidance
-information/covid-19-daily-update-archive.html
9. COVID-19 Timeline. British Foreign Policy Group.
https://bfpg.co.uk/2020/04/
covid-19-timeline/
10. Harper RA, Dhawahir-Scala F, Wilson H, et al. Development and implementation of a Greater Manchester COVID19 Urgent Eyecare Service. Eye 2021;35(3):705-8.
11. Digital Communication between Primary and Secondary Care and Patients. NHS England / Improvement.
https://uk-oa.co.uk/wp-content/uploads/
2020/06/Digital-communications
-for-Eye-Care-May2020.pdf
12. Chloramphenicol. Optometrists’ Formulary. The College of Optometrists.
https://www.college-optometrists.org/
guidance/optometrists-formulary/
chloramphenicol.html
13. Todd D, Bartlett H, Thampy R, et al. Agreement in clinical decision-making between independent prescribing optometrists and consultant ophthalmologists in an emergency eye department. Eye 2020;34(12):2284-94.
14. Easing the bottleneck for IP placements. Optometry Today.
https://www.aop.org.uk/ot/
blogs/2021/05/20/easing-the
-bottleneck-for-ip-placements
15. Kanabar R, Craven W, Wilson H, et al. Evaluation of the Manchester COVID-19 Urgent Eyecare Service (CUES). Eye 2021;36(4):850-858.
16. Siempis T. Urgent Eye Care in the UK Increased demand and challenges for the future. Medical Hypothesis, Discovery and Innovation in Ophthalmology 2014;3(4):103.
17. Independent prescribing in practice. Acuity.
https://www.college-optometrists.org/
acuity-resource/independent
-prescribing-in-practice.html
[All links last accessed June 2021].
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME









