In recent years the surgical treatment of corneal endothelial dystrophy has progressed tremendously. Descemet’s membrane endothelial keratoplasty (DMEK) is the newest iteration in the line of rapid surgical advances that has taken place. However, the previously accepted gold standard prior to DMEK’s appearance as an option, ultra-thin descemet’s membrane endothelial keratoplasty (UT‑DSAEK) has shown exceptional surgical outcomes. The debate is ongoing whether the DMEK should be adopted as the new gold standard given its difficulty and minor improvements in surgical outcomes.
With the publication of three randomised controlled trials (RCTs) comparing DMEK and UT-DSAEK, there is a unique opportunity to critically appraise the literature comparing the two techniques [1-3].
UT-DSAEK is an endothelial keratoplasty technique that seeks to replace the damaged endothelial layer with a thin layer of descemet membrane and endothelium supported by a thin layer of corneal stroma. The technique uses donor grafts that are less than 100 microns. In comparison, DMEK grafts are only 15-20 microns thick as they compose just a single layer of endothelium and Descemet’s membrane. DMEK thus achieves better anatomical correction, which results in better visual acuity observed in RCTs when compared with UT-DSAEK [1-3].
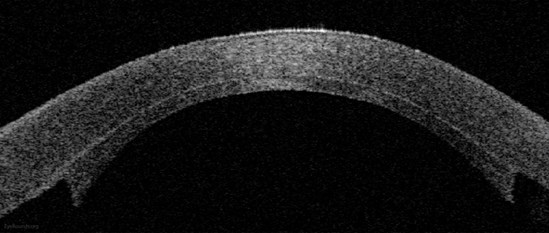
Figure 1: Anterior segment optical coherence tomography demonstrating an attached
DSAEK graft one day after surgery. © EyeRounds.org University of Iowa USA.
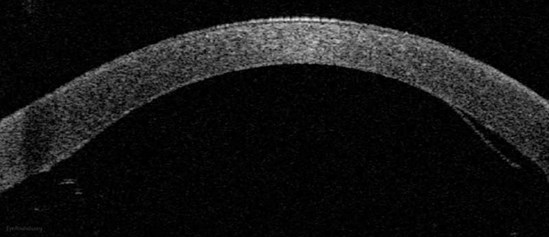
Figure 2: Anterior segment optical coherence tomography demonstrating DMEK
with graft detachment. © EyeRounds.org University of Iowa USA.
However, DSAEK is a significantly less challenging surgery due to the relative thickness of the graft which allows safer graft preparation and easier manipulation in the anterior segment. Consequently, DMEK has a higher complication rate than UT-DSAEK [1,2]. Thus, the question arises, are the visual outcomes in DMEK significantly better over UT-DSAEK to warrant the increased risk of complications?
In the trials published recently, the range of mean visual acuity in the DMEK group at 12 months was 0.04-0.08 logMAR, whereas the range of mean visual acuity at 12 months in the UT-DSAEK group was 0.11-0.16 logMAR. This represents a single line of difference on the visual acuity chart. [1-3] Additionally, patients in the DMEK group achieved faster recovery times along with superior visual acuity at each stage, with the difference being most pronounced earlier in the trial.
However, although DMEK shows clear superiority to UT-DSAEK as assessed by logMAR visual acuity, studies showed that there was no significant difference between the DMEK and UT-DSAEK in patient-reported functional vision as assessed by vision related quality of life (QoL) scores at 12 months [1,3]. These findings were corroborated by fellow eye comparison studies [4].
The trials also reported lower complication rates in the DMEK arm than previously expected, with the Matsou et al. trial showing an almost equal number of complications in either eye. This is potentially because the trials were conducted by a single experienced surgeon who had completed the steep learning curve associated with DMEK. However, both the Dunker and Chamberlain trials showed similar rates of complication, with significantly higher rates in DMEK compared to DSAEK, reflecting the current body of literature [1,2].
“In complicated eyes with poor visualisation, UT-DSAEK may represent a superior choice”
Long-term differences between the two techniques include graft rejection rates and endothelial cell density. It has been generally observed that there is lower endothelial density post-surgery in DMEK patients due to extensive handling of the tissue graft relative to that of UT-DSAEK grafts. However, Dunker et al. reported contrary results and further studies will need to be conducted to determine the difference between either technique [1-3].
UT-DSAEK potentially results in increased rejection rates when compared to DMEK due to increased amount of donor tissue used in UT-DSAEK grafts. Recent studies have shown that rejection rates in UT-DSAEK have improved relative to those experience in DSAEK, with a recent five-year study showing that UT-DSAEK rejection rates are 6.9% at five years [5]. DMEK rejection rates were shown to be 2.6% at five years in a different study [6].
In summary, although DMEK has been shown to provide superior visual acuity and long-term outcomes to UT-DSAEK, these are often not reflected in patient-reported visual outcomes. DMEK is widely perceived to be the hallmark of superior surgical ability, which is why some surgeons may be favouring DMEK over UT-DSAEK rather than deciding on the best treatment option for each individual patient. However, the recent publication of three randomised controlled trials only serves to confirm what we already knew at the start of the decade, which is that in uncomplicated eyes, DMEK should be the technique of choice provided the surgeon has passed the learning curve themselves. In complicated eyes with poor visualisation, UT-DSAEK may represent a superior choice.
References
1. Chamberlain W, Lin CC, Austin A, et al. Descemet endothelial thickness comparison trial: a randomized trial comparing ultrathin descemet stripping automated endothelial keratoplasty with descemet membrane endothelial keratoplasty. Ophthalmology 2019;126(1):19-26.
2. Dunker SL, Dickman MM, Wisse RPL, et al. Descemet membrane endothelial keratoplasty versus ultrathin descemet stripping automated endothelial keratoplasty: a multicenter randomized controlled clinical trial. Ophthalmology 2020;127(9):1152-9.
3. Matsou A, Pujari R, Sarwar H, et al. Microthin descemet stripping automated endothelial keratoplasty versus descemet membrane endothelial keratoplasty: a randomized clinical trial. Cornea 2021;40(9):1117-25.
4. Mencucci R, Favuzza E, Marziali E, et al. Ultrathin descemet stripping automated endothelial keratoplasty versus descemet membrane endothelial keratoplasty: a fellow-eye comparison. Eye Vis (Lond) 2020;7:25.
5. Madi S, Leon P, Nahum Y, et al. Five-year outcomes of ultrathin descemet stripping automated endothelial keratoplasty. Cornea 2019;38(9):1192-7.
6. Price DA, Kelley M, Price FW Jr, Price MO. Five-year graft survival of descemet membrane endothelial keratoplasty (EK) versus descemet stripping EK and the effect of donor sex matching. Ophthalmology 2018;125(10):1508-14.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME





