A study of NHS practice demonstrated significant patient-reported quality-of-life improvements from commonly performed oculoplastic operations: entropion repair, ectropion repair, ptosis repair and dacrocystorhinostomy (DCR) [1].
In recent years, surgical and non-surgical approaches to functional and aesthetic oculoplastic surgery have advanced considerably with the adoption of innovative minimally-invasive techniques, novel procedures and newer technologies. In an interview with Rod McNeil, Consultant Ophthalmic and Oculoplastic Surgeon Mr Raman Malhotra, Corneoplastic Unit, Queen Victoria Hospital NHS Trust, East Grinstead, UK, shares his experience in oculoplastic surgery and highlights practice developments.
“A major trend has been the introduction of non-surgical options in oculoplastic surgery,” explained Mr Malhotra. “The range of off-label uses of botulinum toxin injection (e.g. Botox, Allergan) in ophthalmology has continued to expand. In oculoplastics, botulinum toxin injection may be used for blepharospasm, therapeutic ptosis and watery eyes. Botulinum toxin injection is used to treat crocodile tears after facial palsy, but even more recently, patients who are not suitable for lacrimal surgery often are treated with botulinum toxin injection to the lacrimal gland as a simple non-surgical method to reduce symptoms and maintain quality of life. This trend reflects a greater emphasis on maintaining quality of life and improving the efficiency and effectiveness of care by customising non-surgical interventions to better address individual needs.”
“The use of hyaluronic acid fillers has revolutionised the place for aesthetic eyelid surgery with the development of rejuvenation strategies for lower eyelid bags.”
A report on experience and outcomes using botulinum toxin injection for the treatment of epiphora due to lacrimal outflow obstruction found epiphora completely resolved in one fifth, improved by up to 60-90% in a half and only ‘a little better’ in a further fifth [2]. Temporary bruising and diplopia (lasting two weeks) was reported in 12% (2/17). A review by Singh et al. noted that botulinum toxin injection into the lacrimal gland is a minimally invasive alternative in cases of refractory epiphora secondary to lacrimal drainage disorders [3]. Outcomes from the few studies published were described as encouraging, with transient ptosis the most common reported complication.
Periocular hyaluronic acid filler treatment for volume restoration
Hyaluronic acid is a glycosaminoglycan that is present in body tissues, such as in skin and cartilage. It is able to combine with water and swell when in gel form, causing a smoothing / filling effect. Sources of hyaluronic acid used in dermal fillers can be from bacteria or rooster combs (avian). In some cases, hyaluronic acid used in dermal fillers is chemically modified (crosslinked) to make it last longer in the body. The effects of this material last approximately 12 months but in the periorbital region can last for three to five years.
“The use of hyaluronic acid fillers has revolutionised the place for aesthetic eyelid surgery with the development of rejuvenation strategies for lower eyelid bags,” continued Mr Malhotra. “Restoring volume with filler treatment often achieves a more youthful softer appearance than that obtained following an eyebag operation.
“Hyaluronic acid filler is an effective means of rejuvenating the upper eyelid and is particularly successful in patients with medial / generalised upper eyelid hollowing, or significant post-blepharoplasty upper eyelid show [4]. Surgical experience further confirms the effective use of hyaluronic acid gel (Perlane) for tear-trough rejuvenation as an alternative to lower eyelid surgery [5]. We published results of a consecutive interventional case series (n=198 eyes of 100 patients) using hyaluronic acid gel as a tear-trough filler over an 18-month period [5]. The gel was placed preperiosteally, deep to orbicularis, anterior to the inferior orbital rim, with a mean volume of 0.59ml per eye. High patient satisfaction with minimal complications was noted, with 8% requesting additional hyaluronic acid gel within three months.
“Tear-trough filling offers a minimally-invasive, non-surgical alternative to blepharoplasty, with a reduced risk of complications and minimal recovery time. We use a clear hyaluronic acid gel filler, to create volume and smoother contours. The treatment comprises a series of micro-injections along the line of the hollow. The area is then gently massaged to ensure even distribution of the gel. Results are instant and last well over 12 months.
“Restoring volume in the aging periorbital area with filler treatment has transformed oculoplastic practice, and led to a marked decrease in the need for endoscopic brow lifts. Hollows can make brows extended and heavy, and filler treatment can also effectively address brow temple volume.”
As Lee and Yen note, an understanding of the changes in the upper and lower periocular area due to aging, the meticulous identification of focal hollows, and the precise delivery of filler to these areas can smooth contours and restore a rejuvenated periorbital area [6].
Periocular hyaluronic acid filler treatment is increasingly used as an alternative to traditional surgical procedures for non-aesthetic indications, including lagophthalmos, eyelid malpositions and orbital volume deficiency [7]. Filler injections are minimally invasive, repeatable, titratable and, depending on the product used, may be reversible. Filler treatment may also be used for treating epipheron for volume loss as a non-surgical alternative to orbital implants. Hyaluronic acid fillers provide an effective option for volume restoration with good efficacy and safety and their use reflects the shift to temporary (absorbable) and reversible filler treatment as opposed to permanent fillers such as polymethylmethacrylate beads.
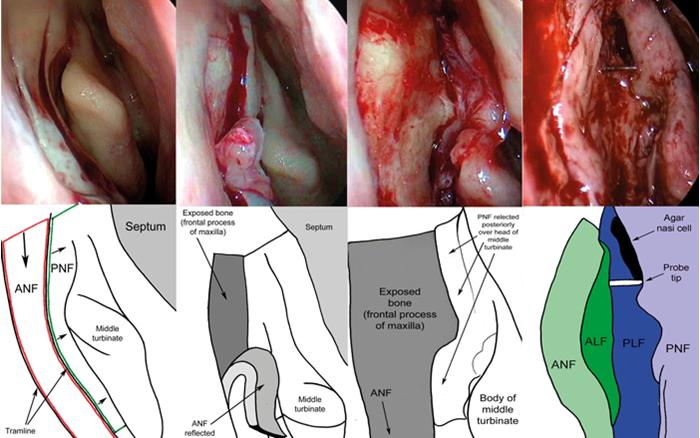
Figure 1: The right nasal cavity view during endoscopic DCR with a large osteotomy, full marsupialisation of the lacrimal sac, creation of mucosal flaps and edge-to-edge mucosal apposition for maximum primary intention healing. No mucosa is excised. A mucosal incision with a small angled crescent blade is made on the lateral nasal wall, at the roof of the nose, at least 8mm above the insertion of the middle turbinate extending down to just below the body of the middle turbinate. A parallel vertical incision made 8mm anterior to this creates the tramline. A superior incision joining the two lines completes the anterior nasal flap (A). The flap is blunt dissected off bone and reflected inferiorly (B). Following reflection of the posterior nasal flap the maxillary bone is more widely exposed (C). Following lacrimal sac marsupialisation, all four flaps are positioned with edge-to-edge apposition. The probe is seen in between the lacrimal flaps (D). Anterior nasal flap (ANF); posterior nasal flap (PNF); anterior lacrimal flap (ALF); posterior lacrimal flap (PLF).
Ptosis correction
A review of surgical management of ptosis and the use of phenylephrine by British Oculoplastic Surgery Society (BOPSS) consultants showed that the majority of consultants will switch from anterior to posterior approach surgery when the phenylephrine test is strongly positive and will also perform bilateral surgery when a contralateral ptosis is induced with phenylephrine [8].
“Müller muscle-conjunctiva resection or white line advancement have become two of the most popular ways of performing ptosis surgery using a posterior approach,” explained Mr Malhotra. “The predictability of correcting height is probably the same as an anterior approach, but the value of posterior approach ptosis surgery is the predictability of the contour.”
Antus et al. recently reported encouraging outcomes from a single-centre case series of patients with severe involutional aponeurotic ptosis undergoing posterior approach white-line advancement ptosis surgery [9]. Involving a mean postoperative follow-up of 28 weeks, success rates were 80.3% overall, 81.5% in the non-visible iris sign (VIS) group and 78% in the VIS group. These outcomes are comparable to, and possibly better than, anterior approach surgery in eyelids with severe ptosis and a VIS.
Favourable long-term outcomes have nonetheless been reported in patients undergoing anterior approach white line advancement for correction of blepharoptosis [10].
Posterior approach levatorpexy
Posterior approach levatorpexy is a safe and effective procedure for correction of congenital ptosis. This minimally invasive surgical procedure involves exposing the posterior surface of the levator muscle through a transconjunctival approach. The levator muscle is advanced and plicated using a suture passed through its posterior surface, partial-thickness, to tarsal plate and tied on the skin. No tissue (conjunctiva, Muller’s muscle, levator) are excised [11].
“We undertook a retrospective review of levatorpexy for congenital ptosis with reduced levator function and found posterior approach levatorpexy to be a useful first-line choice for congenital ptosis for all ranges of levator function [12]. It is popular among parents due to avoidance of a skin incision or any resection and no excision of tissue. In my mind, I cannot see a justification for doing an anterior approach for congenital ptosis repair when similar outcomes can be achieved using a posterior approach without the need for skin incision or tissue removal.”
Platinum chains for upper eyelid loading
“Over the past five years, our Corneoplastic Unit and Trust have expanded considerably and we are now one of the largest facial nerve palsy services in the UK. The big mantra is achieving effective closure and a natural appearance for eyelid and facial appearance. This is particularly important for lower eyelid position, upper eyelid appearance, and the shape of the eye. My preference is to use platinum chains instead of gold weights for upper eyelid loading in the management of lagophthalmos. Platinum is denser than gold and therefore less bulky. Moreover, platinum chains contour the eyelid better than gold weights.”
A review of late outcomes over a 10-year period to 2013 showed that gold weights were associated with a higher rate of complications and twice more likely to require long-term revision surgery compared with platinum chains [13]. Gold weights had a significantly higher rate of weight prominence and migration compared with platinum chains.
“There are now many more procedures available for achieving an aesthetically natural appearance. For facial palsy, recession of eyelid retractors helps to elevate the lower eyelid to address eyelid malposition. Most of the time I am recessing retractors in ectropion surgery, particularly for facial palsy. I would hope surgeons start questioning that old dogma of advancing or plicating retractors, as this contributes to retraction long term. Also, by using trans (or retro) caruncular medial eyelid fixation approaches I also rarely need to perform medial canthoplasties that create a rounded canthus.
“We also have an established multidisciplinary approach for facial palsy, with a large physiotherapy support service helping transform patient outcomes through to rehabilitation and recovery and preventing the development and impact of synkinesis.”
Endoscopic lacrimal surgery
Powered-endoscopic DCR is an endonasal-approach procedure used to bypass the nasolacrimal duct. Endoscopic DCR is indicated for patients with lacrimal sac obstruction or nasolacrimal duct obstruction (NLDO). NLDO is common, and presenting symptoms include watering of the eye and dacryocystitis (infection) [14]. Endoscopic DCR is usually considered for patients who have been refractory to conventional treatment such as warm compresses, massage and probing of the nasolacrimal duct. If NLDO is left untreated, the symptoms persist and may be distressing for the patient.
Mr Malhotra continued: “Outcomes from a multicentre series demonstrate that DCR is a safe operation, with an overall success rate of 90% for paediatric nasolacrimal duct obstruction. Complete symptom resolution was observed in 78% (90/116), significant improvement in 12% (14/116), partial improvement in 2% (2/116) [15]. The main advantage of powered-type endoscopic DCR over external DCR is faster recovery rate without skin incision or muscle trauma. External DCR involving nasal incision is associated with a slight risk of permanently weakening the blink.
“There is still a role for external DCR in appropriately selected patients, for example in those who have a very narrow nasal space and who are therefore unsuitable for septoplasty, those not suitable for a general anaesthetic, or occasionally in those with canalicular disease. Other than that, an endonasal approach to DCR is definitely the procedure of choice and is now established practice. It has to be carried out according to the surgical principles of full sac exposure, complete osteotomy and creating nasal flaps for primary intention mucosal healing. A practice audit of my endonasal DCR cases performed over the previous two years showed, in the absence of patients with canalicular disease, a 100% success rate.”
Simultaneous nasal procedures may be required in a significant proportion of patients undergoing endoscopic DCR [16]. A multicentre evaluation reported that 14.1% of a total cohort of 576 patients required a concomitant endonasal procedure during endoscopic DCR (11.9% required septoplasty, 1.5% middle turbinate surgery and 0.34% polypectomy).
Thyroid eye disease
Most cases of thyroid eye disease are managed effectively in the active inflammatory phase with systemic corticosteroids, and intervenous pulsed methyl predinisolone regimes have now transformed steroid management, reducing steroid-related side effects in these patients. Orbital decompression nowadays is commonly performed in the inactive phase for non-sight threatening indications such as exophthalmos-related exposure or congestion in addition to sight-threatening compressive optic neuropathy. Immunosuppression in the active inflammatory phase of thyroid eye disease is paramount in order to reduce the long-term sequelae of acute inflammation [17].
Antiproliferative immunosuppression with azathioprine may possibly confer additional benefit in adults with active moderate-to-severe thyroid eye disease associated with proptosis or ocular motility restriction, according to results from CIRTED, a multicentre, double-blind, randomised controlled trial conducted at six UK centres [18].
“Perhaps the most exciting breakthrough is the inhibition of the insulin-like growth factor I receptor (IGF-IR) as a new therapeutic strategy to attenuate the underlying autoimmune pathogenesis of thyroid-associated ophthalmopathy,” continued Mr Malhotra [19]. Teprotumumab is a human monoclonal antibody inhibitor of IGF-IR that blocks the induction of proinflammatory cytokines. Results of a multicentre, randomised, placebo-controlled trial demonstrated that teprotumumab was more effective than placebo in reducing proptosis and the Clinical Activity Score [19]. This may prove to be a major change in the way active thyroid eye disease will be managed in the near future.
Expansion of advanced oculoplastic cadaveric courses
Brow lifts, blepharoplasty, ptosis correction, removal of benign eyelid or skin lesions and procedures to treat watering eyes are often included on lists of procedures for which Clinical Commissioning Groups do not routinely provide funding. According to the Royal College of Ophthalmologists, prompt assessment and treatment is needed when there is a likelihood of malignancy, or where eyelid malposition threatens the ocular surface. There should also be provision for treatment where brow droop or ptosis reduce the field of vision to the point where the ability to drive is compromised.
Oculoplastic centres should be photographing all cases pre- and postoperatively in a standardised manner and record baseline and post-treatment visual acuity, said Mr Malhotra. “Many oculoplastic procedures now require low priority applications for funding and oculoplastic surgery case numbers overall in NHS-funded care have declined as a result. Ophthalmic trainees often voice concerns that they are not getting sufficient exposure to ptosis surgery cases for training purposes. Training under supervision in ptosis surgery, while no longer a curriculum requirement for general ophthalmologists, is a good exercise in developing global skills in oculoplastics.”
Oculoplastic cadaveric courses offer advanced surgical training opportunities for oculoplastic fellows, senior trainees with an interest in oculoplastic surgery and consultants with an interest in oculoplastic surgery. The Manchester Oculoplastic, Lacrimal and Orbital Dissection Course, at Central Manchester University Hospitals NHS Foundation Trust, is hugely popular and usually oversubscribed. It is one of the most technologically advanced surgical skills labs in the UK. The course is focused on anatomy, dissection and surgical techniques, with a high expert faculty to delegate ratio. Course contents include enucleation, evisceration and exenteration, techniques that all trainees should master. Similar courses exist nationwide, for example, the Coventry Ophthalmic Surgery Skills Cadaver Course at University Hospitals Coventry and Warwickshire NHS Trust. Details of these courses can be found on the BOPSS website (www.bopss.co.uk).
References
1. Smith HB, Jyothi SB, Mahroo OA, et al. Patient-reported benefit from oculoplastic surgery. Eye (Lond) 2012;26(11):1418-23.
2. Ziahosseini K, Al-Abbadi Z, Malhotra R. Botulinum toxin injection for the treatment of epiphora in lacrimal outflow obstruction. Eye (Lond) 2015;29(5):656-61.
3. Singh S, Ali MJ, Paulsen F. A review on use of botulinum toxin for intractable lacrimal drainage disorders. Int Ophthalmol 2017 [Epub ahead of print].
4. Morley AM, Taban M, Malhotra R, Goldberg RA. Use of hyaluronic Acid gel for upper eyelid filling and contouring. Ophthal Plast Reconstr Surg 2009;25(6):440-4.
5. Morley AM, Malhotra R. Use of hyaluronic acid filler for tear-trough rejuvenation as an alternative to lower eyelid surgery. Ophthal Plast Reconstr Surg 2011;27(2):69-73.
6. Lee S, Yen MT. Nonsurgical rejuvenation of the eyelids with hyaluronic acid gel injections. Semin Plast Surg 2017;31(1):17-21.
7. Tan P, Kwong TQ, Malhotra R. Non-aesthetic indications for periocular hyaluronic acid filler treatment: a review. Br J Ophthalmol 2017 [Epub ahead of print].
8. Mota PM, Norris JH. Review on surgical management of ptosis and the use of phenylephrine: A national survey of British Oculoplastic Surgery Society (BOPSS) UK Consultants. Orbit 2016;35(6):339-42.
9. Antus Z, Salam A, Horvath E, Malhotra R. Outcomes for severe aponeurotic ptosis using posterior approach white-line advancement ptosis surgery. Eye (Lond) 2018;32(1):81-6.
10. Schulz CB, Nicholson R, Penwarden A, Parkin B. Anterior approach white line advancement: technique and long-term outcomes in the correction of blepharoptosis. Eye (Lond) 2017;31(12):1716-23.
11. Al-Abbadi Z, Sagili S, Malhotra R. Outcomes of posterior-approach ‘levatorpexy’ in congenital ptosis repair. Br J Ophthalmol 2014;98(12):1686-90.
12. Feldman I, Brusasco L, Malhotra R. Improving outcomes of posterior approach levatorpexy for congenital ptosis with reduced levator function. Ophthal Plast Reconstr Surg 2018 [Epub ahead of print].
13. Siah WF, Nagendran S, Tan P, et al. Late outcomes of gold weights and platinum chains for upper eyelid loading. Br J Ophthalmol 2018;102(2):164-8.
14. National Institute for Health and Care Excellence. Endoscopic dacryocystorhinostomy Interventional procedures guidance 113. 2005.
https://www.nice.org.uk/guidance/ipg113
Last accessed May 2018.
15. Chan W, Wilcsek G, Ghabrial R, et al. Pediatric endonasal dacryocystorhinostomy: A multicenter series of 116 cases. Orbit 2017;36(5):311-6.
16. Figueira E, Al Abbadi Z, Malhotra R, et al. Frequency of simultaneous nasal procedures in endoscopic dacryocystorhinostomy. Ophthal Plast Reconstr Surg 2014;30(1):40-3.
17. Verity DH, Rose GE. Acute thyroid eye disease (TED): principles of medical and surgical management. Eye (Lond) 2013;27(3):308-19.
18. Rajendram R, Taylor PN, Wilson VJ, et al. Combined immunosuppression and radiotherapy in thyroid eye disease (CIRTED): a multicentre, 2 × 2 factorial, double-blind, randomised controlled trial. Lancet Diabetes Endocrinol 2018;6(4):299-309.
19. Smith TJ, Kahaly GJ, Ezra DG. Teprotumumab for thyroid-associated ophthalmopathy. N Engl J Med 2017;376(18):1748-61.
TAKE HOME MESSAGE
-
Non-surgical options in oculoplastic surgery have expanded significantly
-
Restoring volume in the ageing periorbital area with hyaluronic acid gel filler treatment has transformed oculoplastic practice
-
Müller muscle-conjunctiva resection or white line advancement have become two of the most popular ways of performing ptosis surgery using a posterior approach
-
Posterior approach levatorpexy is a safe and effective procedure for correction of congenital ptosis
-
Platinum chains contour the eyelid better than gold weights
-
An endonasal approach to dacryocystorhinostomy is the procedure of choice
-
Inhibition of the insulin-like growth factor I receptor (IGF-IR) represents a promising new therapeutic strategy for the management of active thyroid eye disease
COMMENTS ARE WELCOME