Management options and outcomes in glaucoma practice were reviewed at the 7th Moorfields International Glaucoma Symposium, held in London on 24 January 2015. This article summarises perspectives from international glaucoma specialists on debated issues in topical therapy, glaucoma surgery, diagnostic practice, public health and service delivery.
Reassessing glaucoma drops (chairs Peng Tee Khaw and Fiona Spencer)
Alex J Shortt noted that the prevalence of ocular surface disease (OSD) is over-represented in glaucoma patients but is under-diagnosed and poorly treated, leading potentially to poor treatment compliance (Table 1) [1].

Ocular surface symptoms experienced by patients on preserved eye drop treatment represent a major barrier to compliance in glaucoma treatment [2]. All components of glaucoma eye drops have the potential for toxicity but some compounds are disproportionately toxic [3]. Mr Shortt raised concerns about glaucoma medicines preserved with benzalkonium chloride (BAK), cautioning that direct BAK toxicity disturbs ocular surface homeostasis, leading to cell death, corneal vascularisation, inhibition of healing and potentially surgical failure. Benzalkonium chloride is highly toxic to trabecular meshwork cells.
Withdrawing the use of BAK-preserved topical medicines may allow normal ocular surface homeostasis to recover; if not, full assessment and treatment of OSD may prove helpful. There is evidence that preservative-free glaucoma medications lead to better intraocular pressure (IOP) control overall due to improved compliance and adherence to prescribed treatment regimens.
Gus Gazzard reviewed initial treatment options for glaucoma. Medical treatment for glaucoma works well for many patients, but barriers include low overall compliance due to complex dosing schedules and local or systemic side-effects, non-responder rates, tachyphylaxis, and costs of repeat clinic visits, treatment switches and often a need for multiple drug regimens. Alternative initial treatment options for glaucoma include different drug delivery systems, selective laser trabeculoplasty (SLT) and early trabeculectomy.
In routine practice, SLT is used most often as a second- or third-line treatment for glaucoma, while experience indicates less dramatic response rates than those observed in the published literature. The LiGHT trial, evaluating the efficacy of laser in glaucoma and ocular hypertension (OH), will provide further evidence regarding preferred first-line therapy in treatment naïve patients with mild and moderate open-angle glaucoma (OAG) or OH. The Treatment of Advanced Glaucoma Study (TAGS) is a multicentre randomised controlled trial currently in progress comparing primary medical treatment with primary augmented trabeculectomy for patients with newly diagnosed advanced glaucoma. TAGS will assess relative effectiveness, safety and costs in routine practice, with the primary outcome evaluated at 24 months.
The selection of primary treatment depends largely on disease staging (mild, moderate or severe, unilateral or bilateral blindness) and other individual patient characteristics or preferences.
Alternative drug delivery technologies
Patients may experience significant side-effects from topical glaucoma treatments, and poor treatment persistence and adherence is an underestimated concern in a large proportion of patients, explained Jonathan Clarke. Elderly people often struggle with drop instillation technique, and discontinuation of therapy is common. Nordstrom et al. found substantially better overall treatment compliance with prostaglandins than with other hypotensive drug classes [4].
Other ophthalmic drug delivery systems under investigation include a range of surgical implants and both passive and active drug release inserts (Figure 1).

Source: Kassam F, et al. Clin Exp Optom 2013;96:577-80.
Figure 1: Illustration of several novel investigational drug delivery platforms being tested as potential intraocular pressure-lowering treatment modalities.
Delivery via the subconjunctival route is being tested, for example using a timolol-loaded microfilm drug delivery system. Concerns remain over patient acceptance and overall ocular safety, for example with regard to nasolacrimal duct changes with chronic use of drug eluting devices.
Security of vision-preserving benefit using prostaglandin analogue latanoprost
Topical medication remains favoured as primary treatment for glaucoma and OH, largely because of the immediate hypotensive effect achieved with drops and an ability to titrate the treatment, explained Rupert Bourne (Hinchingbrooke Hospital, Huntingdon). Maximum pressure lowering is achieved within the first three to five weeks of treatment commencement on prostaglandin therapy.
Two-year findings from United Kingdom Glaucoma Treatment Study (UKGTS) show longer preservation of the visual field in newly diagnosed and previously untreated OAG patients (with mild to moderate glaucoma) given prostaglandin analogue latanoprost compared with those receiving placebo (adjusted hazard ratio 0·44, 95% confidence interval 0·28-0·69; p=0·0003) [5]. The data demonstrate the vision-preserving benefit of topical prostaglandin analogues and ultimately the patient benefit of lowering IOP, evident over a relatively short observation period.
Opportunities to improve adherence with topical medication
Severe dry eye and the toxic effects of preserved drops may undermine the use of intraocular pressure-lowering medication as prescribed, reiterated Mr Bourne. The toxic effects of preservatives are dose dependent and cumulative. Short-term BAK administration, for example with BAK-preserved timolol drops, penetrates the back of the eye and produces inflammation at the level of the anterior chamber, as well as deleterious ocular surface effects [6]. Benzalkonium chloride may contribute to apparent loss of clinical efficacy with monotherapy, with close to half of glaucoma patients requiring multiple medications for effective IOP control.
Because of the known toxic and pro-inflammatory effects of preserved eye drops and BAK in particular, preservative free compounds are sometimes preferred initial therapy for glaucoma patients and for other individuals who require chronic ocular drug administration. Appropriate patient populations include those with a known allergy to the preservative, Sjögren syndrome or severe dry eye disease (stage 3,4), atopic dermatitis and rosacea, and children; in addition, those with clinically relevant dry eye disease (stage 2), requiring concomitant topical therapy, long life-expectancy, blepharitis or meibomian gland dysfunction (MGD), intolerance to the preservative, or at high risk of need for surgical intervention [7].
In addition to avoiding BAK, active education and instruction on correct drop instillation technique may help improve adherence and treatment outcomes with intraocular pressure-lowering eye drops [8].
Glaucoma surgery (chairs Sheng Lim and John Brookes)
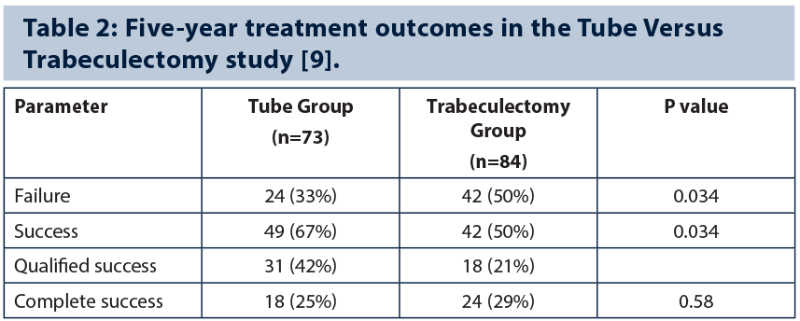
Failed trabeculectomy is not an uncommon challenge. Five-year treatment outcomes in the Tube Versus Trabeculectomy (TVT) Study demonstrate a higher success rate with tube shunt surgery compared to trabeculectomy with mitomycin C (MMC) in patients with uncontrolled glaucoma and previous ocular surgery (Table 2) [9]. Investigators observed a cumulative probability of failure of 29.8% in the tube group and 46.9% in the trabeculectomy group during five years’ follow-up. The TVT study found that tube shunt surgery and trabeculectomy have similar efficacy in eyes with previous conjunctival surgery, while tube surgery had fewer high IOP failures and fewer low IOP failures than trabeculectomy, implying better predictability.
Indications for glaucoma drainage tube surgery include situations where trabeculectomy has an established poor record of success, commented Keith Barton. Glaucoma drainage implant surgery is suitable in most complex glaucomas, in patients with uncontrolled glaucoma who have had previous trabeculectomy and / or cataract extraction with intraocular lens (IOL) implantation, and in patients whose sole priority is to get off long-term topical medications. The postoperative course tends to be more predictable than that achieved with repeat trabeculectomy surgery, while results from the TVT study confound the myth that low pressures are not achievable with tube shunt surgery.
The Ahmed Baerveldt Comparison (ABC) Study found similar rates of surgical success over five years following implantation with either a Ahmed Glaucoma Valve or a Baerveldt Glaucoma Implant, although the latter produced greater IOP reduction [10]. Correct tube shunt placement remains paramount.
Bleb salvage through needling or revision, repeat filtering surgery and glaucoma drainage device surgery are all valid surgical approaches following trabeculectomy failure, but the order of interventions is important, explained Anthony King. The initial step should be to restore function to a trabeculectomy bleb and thereby reduce or control IOP, with drainage device surgery reserved as a last resort. Needling revision with adjunctive MMC can effectively revive flat filtering blebs and appears to be safe for the corneal endothelium. Results from the TVT study are not sufficient alone to justify immediate glaucoma drainage tube surgery in failed trabeculectomy cases. Reasonable outcomes are achievable with several different surgical options, but it is uncertain which if any approach is best due to a lack of comparative evaluations.
Next-generation microinvasive glaucoma surgery procedures
Evolving miroinvasive glaucoma surgery (MIGS) techniques and clinical data were reviewed by Ike K Ahmed (University of Toronto, Canada). Novel devices include iStent, the Hydrus intracanalicular microstent, suprachoroidal shunts such as the CyPass Micro-Stent and subconjunctival microstents. Early clinical results evaluating the AqueSys XEN Gel implant, which involves an ab interno gel-stent external bleb forming procedure, suggest ‘trabeculectomy-like’ pressure reduction outcomes. Minimally traumatic interventional approaches continue to evolve and entail a stepwise approach, permitting earlier intervention using MIGS devices for mild to moderate glaucoma [11]. Microinvasive glaucoma surgery is routinely combined with phacoemulsification in appropriate cases, while long tube shunts are still necessary for refractory surgical cases.
Challenging surgical cases and learning points
Uveitic glaucoma
Keith Martin (Addenbrooke’s Hospital, Cambridge) presented strategies for the surgical management of uveitic glaucoma, noting that secondary glaucoma occurs in around 10-20% of uveitis patients. Treat the uveitis and address the cause of IOP elevation, recommended Mr Martin. Laser iridotomy or surgical iridectomy are indicated in eyes with pupillary block, although laser procedures in uveitic eyes are difficult and have a high early failure rate, especially in pigmented eyes. Trabeculectomy is a reasonable option in selected uveitic patients: good control of flow at time of surgery and meticulous conjunctival closure are important, as is careful postoperative management. Preservative-free steroids are recommended post-surgery. Primary tube surgery may be considered in selected high-risk uveitic glaucoma patients.
Keratoprosthesis (KPro) surgery
Keratoprosthesis implantation involves life-changing surgery in patients with multiple failed corneal grafts and those at high risk of repeat graft failure. Integrated clinical management and planning is needed, noted Nick Strouthidis, with Moorfields having established a combined cornea / glaucoma KPro clinic. Results of a retrospective note review of 26 consecutive cases (11 with pre-existing glaucoma) treated with keratoprosthesis surgery at Moorfields illustrate the potential for blinding glaucoma complications. Patients nonetheless can secure good useful vision from KPro and it is often the only option available. Counselling against surgery is advisable in higher risk patients, such as those with pre-existing hypotony or end-stage glaucoma.
“It is important not to miss a chance to make a better diagnosis.”
Drainage tube failures
Winifred Nolan discussed management strategies for glaucoma patients who experience progression following previous drainage tube surgery. For early failure, options include: flush tube, needle plate, reposition and extend; capsule excision; and topical medications. A second tube positioned superonasal or inferiorly may be considered for late failure cases. When there is progressive visual field loss and apparently normal pressure levels, cyclodiode laser treatment may be considered.
Angle-closure glaucoma
Paul J Foster addressed interventions in a series of challenging primary angle-closure glaucoma (PACG) case presentations. Avoiding trabeculectomy in PACG is wise, especially in Caucasian patients, consider lens implant options carefully and beware patients with thick sclera as well as potential biometry errors in small eyes with angle-closure glaucoma (ACG). Panel discussions highlighted clinical trial data that demonstrate phacoemulsification alone can effectively lower IOP long-term in eyes with PACG and coexisting cataract, while topical prostaglandin analogue therapy is effective in reducing the IOP of patients with angle-closure glaucoma. Trabeculectomy may prove effective in pseudophakic ACG patients.
The diagnostic dilemma (chairs Nick Strouthidis and Philip Bloom)
When to discharge from active glaucoma care
Questionable referrals on IOP measurement alone and high first-visit discharge rates present ongoing issues in effective glaucoma service delivery, explained Ananth C Viswanathan.
Experience in the UK indicates a steep climb in the first-visit discharge rate since issuance of glaucoma guidelines by the National Institute for Health and Care Excellence (NICE) in 2009 [12]. An overemphasis on elevated IOP as a criterion for referral has led many centres to develop glaucoma referral refinement schemes to help prioritise assessment of high- and low-risk suspects. Clinical guidelines advise that referral on IOP alone is based on repeated measurements greater than 21mmHg, ideally using Goldmann applanation tonometry. A study of outcomes of glaucoma referrals across Europe shows that overall, 35.2% of referrals had no ocular pathology; country-specific rates were 40% in a UK centre, 16% in Italy and 60% in Greece [Founti et al. ARVO 2015; abstract submission].
Guidelines from NICE state that people should be discharged to community optometric care if there is no detected change in clinical assessment parameters (IOP, optic nerve head and visual field) after three to five years, or before if confirmed normal.
Debate: optic disc imaging in routine glaucoma practice
Optic disc imaging is useful only rarely in real-world glaucoma practice, argued Philip Bloom (Western Eye Hospital, London). That said, image quality is important for diagnostic and follow-up management, although patients with peculiar non-pathological features may produce misleading outcomes. Normative databases are limited, only useful for general probability analysis and may not be representative of all patient populations. Diagnostic difficulties may arise due to the large variations seen in normal disc appearance. Clinical judgment and regular functional assessment of visual fields are therefore crucial.
Andrew Tatham (Princess Alexandra Eye Pavilion, Edinburgh) stressed the importance of optic disc imaging in early diagnosis, for assessing progression and risk of visual loss, complementing visual field analysis and allowing more efficient ways of working. Imaging helps detect early glaucomatous disease and to triage referrals made on the basis of suspicious discs, but its greatest value is in progression monitoring and the added value provided alongside visual field assessment [13].
Structural changes are predictive of visual loss in established glaucoma and therefore patients with glaucoma or suspected glaucoma should be assessed with a combination of structural and functional tests. Miki et al. reported that a 1-μm/year faster rate of retinal nerve fibre layer (RNFL) thickness loss corresponded to a 2.05-times higher risk of developing visual field damage, in a study of glaucoma suspects with a median follow-up of 2.2 years [14].
What not to miss in the clinic
Jeffrey M Liebmann (Columbia University Medical Center, New York, USA) emphasised practice tips in the clinical management of glaucoma to enhance patient care. It is important not to miss a chance to make a better diagnosis (e.g. gonioscopy is performed on all primary OAG patients), high risk features for progression (e.g. disc haemorrhage, requiring continuous surveillance), significant progression (monitor structural change via assessments of disc topography, RNFL and disc haemorrhage), central visual field loss (10-2 test should be routine), the impact of increasing life-expectancy on lifetime risk of blindness, or a good screening opportunity.

Failure to diagnose low tension glaucoma results in late diagnosis, more difficult treatment options and poorer outcomes (Table 3). More than half of open-angle glaucoma patients may have a statistically normal IOP reading, so it is vital to examine the optic disc. Increasing life-expectancy raises the risk of not only disability but also of blindness from glaucoma. There is notable morbidity associated with even small amounts of visual function decline. These considerations support renewed emphasis on early diagnosis and prompt treatment of glaucoma.
Learning new surgical techniques, (chairs Julián García Feijóo and Dilani Siriwardena)
Julián García Feijóo (Universidad Complutense de Madrid, Spain) presented practical recommendations on mastering microinvasive glaucoma surgery techniques and related surgical complications. Subconjunctival implants may play an important role in the conventional treatment algorithm for glaucoma, particularly when a target IOP in the low teens is required. The goal is to increase the outflow enhancing the physiological drainage pathways. Suprachoroidal devices may offer potential for treatment of more advanced cases. Surgeons should practise using newer instrumentation and bimanual techniques, and follow manufacturer and / or reference surgeon recommendations. Ophthalmic surgeons should master gonioscopy, use a goniolens at the end of cataract procedures and always check implant position before completing a case. Also, surgeon positioning is important to ensure good angle visualisation.
Public health and service delivery (chairs Winifred Nolan and Richard Wormald)
Teleglaucoma – from a distance, it’s here to stay
Teleglaucoma is about building subspecialty and institutional capacity, with more case detection of high risk characteristics, explained Karim F Damji (University of Alberta, Canada). Early detection and treatment result in improved prognosis, but there’s a need to improve access and efficiency of care and teleglaucoma is an effective screening tool for glaucoma. It can accurately discriminate between screen test results with greater odds for positive cases and study data show teleglaucoma detects more cases of glaucoma than in-person or in-house examination [15]. Teleglaucoma allows collaborative care, faster access for patient care, and more efficient assessments through virtual consultation, while patient satisfaction is good to high.
Outcomes from a collaborative care patient-centred teleglaucoma programme in Northern Alberta, evaluating 247 patient referrals from 2008 to 2012, show that most could be managed through distance collaboration [16]. A prospective comparative study showed significant improvements in mean access time and cycle time for patients seen through a teleglaucoma programme compared to those seen using a conventional in-person physician examination (Table 4) [17]. However, certain patient subgroups may not be well suited to a ‘virtual’ care model, for example individuals with advanced or advancing glaucoma damage, extremely high eye pressure (>35 mmHg), or with features suggestive of glaucoma other than primary OAG.
Used correctly, teleglaucoma assessment can add enormously to improving management pathways in glaucoma care, observed Ian Murdoch. However, the greatest benefit is in remote monitoring of patients with established glaucoma. As there is no single test or battery of tests that can consistently and reliably diagnose glaucomas, clinical nous is necessary when interpreting test results. In diagnosing change in an existing patient case, face-to-face examination is preferred for repeat angle assessment, anterior segment assessment and disc evaluation. Investigations evaluating the positive and negative predictive power of teleglaucoma schemes for the detection and monitoring of change in glaucoma are needed [18].

Source: Kassam F, et al. Clin Exp Optom 2013;96:577-80.
Figure 2: Guiding principles for collaborative care and teleglaucoma models.
Collaborative care involving allied healthcare professionals welcomed
Community refinement of glaucoma referrals can reduce the number of suspect glaucoma cases referred to secondary care, explained Fiona Spencer (Manchester Royal Eye Hospital, Manchester). NICE guidelines are useful in the development of collaborative care models involving optometrists, many of whom are independent prescribers who can initiate treatment where needed. Guidelines from NICE confirm key competencies required of suitably trained healthcare professionals involved in diagnosis of ocular hypertension, suspected chronic OAG and formulation of a management plan. Successful collaboration with allied healthcare professionals calls for early engagement, development of team-based decision-making and independence (Figure 2). It is worthwhile considering a stepwise development approach or introduce tiered clinics for patient sub-groups classified by need and risk level.
Strategies for reducing glaucoma blindness
Despite diagnostic and treatment advances, a large proportion of glaucoma patients still progress to blindness due to either late diagnosis or incomplete understanding of the condition, noted Ramanjit Sihota (R P Centre for Ophthalmic Services, New Delhi, India). Studies show that blindness from glaucoma can be reduced but not eradicated entirely. However, greater public awareness and broader screening can improve rates of early diagnosis. Lower ‘target pressures’ for all glaucomas, more affordable medications, treatment emphasis on the ‘better’ eye to preserve complete vision, and early surgical intervention may help to further slow progression rates. More too can be done to help prevent angle-closure glaucoma. There is a need for objective progression assessment as well as virtual monitoring for remote communities.
Interventions focused on prevention, long-acting drug delivery technologies, gene and stem cell therapy, as well as immunotherapy, may provide alternative options in the future for control of glaucomatous vision loss.
References
1. Leung EW, Medeiros FA, Weinreb RN. Prevalence of ocular surface disease in glaucoma patients. J Glaucoma 2008;17(5):350-5.
2. Michée S, Brignole-Baudouin F, Riancho L, et al. Effects of benzalkonium chloride on THP-1 differentiated macrophages in vitro. PLoS One 2013;8(8):e72459.
3. Saarinen-Savolainen P, Järvinen T, Araki-Sasaki K, et al. Evaluation of cytotoxicity of various ophthalmic drugs, eye drop excipients and cyclodextrins in an immortalized human corneal epithelial cell line. Pharm Res 1998;15(8):1275-80.
4. Nordstrom BL, Friedman DS, Mozaffari E, et al. Persistence and adherence with topical glaucoma therapy. Am J Ophthalmol 2005;140(4):598-606.
5. Garway-Heath DF, Crabb DP, Bunce C. Latanoprost for open-angle glaucoma (UKGTS): a randomised, multicentre, placebo-controlled trial. Lancet 2014 Dec [Epub ahead of print].
6. Stevens AM, Kestelyn PA, De Bacquer D, Kestelyn PG. Benzalkonium chloride induces anterior chamber inflammation in previously untreated patients with ocular hypertension as measured by flare meter: a randomized clinical trial. Acta Ophthalmol 2012;90(3):e221-4.
7. Stalmans I, Sunaric Mégevand G, Cordeiro MF, et al. Preservative-free treatment in glaucoma: who, when, and why. Eur J Ophthalmol 2013;23(4):518-25.
8. Tatham AJ, Sarodia U, Gatrad F, Awan A. Eye drop instillation technique in patients with glaucoma. Eye (Lond) 2013;27(11):1293-8.
9. Gedde SJ, Schiffman JC, Feuer WJ, et al; Tube versus Trabeculectomy Study Group. Treatment outcomes in the Tube Versus Trabeculectomy (TVT) study after five years of follow-up. Am J Ophthalmol 2012;153(5):789-803.
10. Budenz DL, Barton K, Gedde SJ, et al; Ahmed Baerveldt Comparison Study. Five-year treatment outcomes in the Ahmed Baerveldt Comparison Study. Ophthalmology 2015;122(2):308-16.
11. Saheb H, Ahmed II. Micro-invasive glaucoma surgery: current perspectives and future directions. Curr Opin Ophthalmol 2012;23(2):96-104.
12. Ratnarajan G, Newsom W, Vernon SA, et al. The effectiveness of schemes that refine referrals between primary and secondary care--the UK experience with glaucoma referrals: the Health Innovation & Education Cluster (HIEC) Glaucoma Pathways Project. BMJ Open 2013;3:e002715.
13. Medeiros FA, Zangwill LM, Girkin CA, et al. Combining structural and functional measurements to improve estimates of rates of glaucomatous progression. Am J Ophthalmol 2012;153(6):1197-205.
14. Miki A, Medeiros FA, Weinreb RN, et al. Rates of retinal nerve fiber layer thinning in glaucoma suspect eyes. Ophthalmology 2014;121(7):1350-8.
15. Thomas SM, Jeyaraman M, Hodge WG, et al. The effectiveness of teleglaucoma versus in-patient examination for glaucoma screening: a systematic review and meta-analysis. PLoS One 2014;9(12):e113779.
16. Verma S, Arora S, Kassam F, et al. Northern Alberta remote teleglaucoma program: clinical outcomes and patient disposition. Can J Ophthalmol 2014;49(2):135-40.
17. Arora S, Rudnisky CJ, Damji KF. Improved access and cycle time with an “in-house” patient-centered teleglaucoma program versus traditional in-person assessment. Telemed J E Health 2014;20(5):439-45.
18. Strouthidis NG, Chandrasekharan G, Diamond JP, Murdoch IE. Teleglaucoma: ready to go? Br J Ophthalmol 2014;98(12):1605-11.
Acknowledgements:
The article is based on presentations and discussions during the 7th Moorfields International Glaucoma Symposium, 24 January 2015, Royal College of Physicians, London, UK. Symposium planning and programme directors Keith Barton, Winifred Nolan and Nick Strouthidis reviewed the draft manuscript and approved the final version for publication submission. The meeting was supported by an educational grant from Théa Pharmaceuticals. Medical writing support was provided by Rod A McNeil, BA, MBA, which was funded by Théa Pharmaceuticals.
Decision-making in the glaucoma clinic: practical tips on what not to miss:
-
A chance to make a better diagnosis
-
High risk features for glaucomatous progression
-
Significant progression
-
Central visual field loss (10˚), which directly impacts quality of life
-
Impact of increasing life-expectancy on lifetime risk of glaucoma blindness
-
A good screening opportunity.
Declaration of Competing Interests
Keith Barton has received lecture honoraria from Allergan and Pfizer, and educational grants / research funding from AMO, New World Medical, Alcon, Merck, Allergan and Refocus. He is on the advisory boards for Glaukos, Alcon, Merck, Kowa, Amakem, Théa, Alimera, Refocus and Ivantis, and works as a consultant for Alcon, AqueSys, Ivantis, Refocus and Carl Zeiss Meditec. He also holds shares in AqueSys, Ophthalmic Implants (PTE) Ltd, Vision Futures (UK) Ltd (Director), London Claremont Clinic Ltd (Director) and Vision Medical Events Ltd (Director).
COMMENTS ARE WELCOME