
Recurrent corneal erosion syndrome is a common, recurrent condition caused by abnormal epithelial adhesion to the underlying basal lamina. Spontaneous breakdown of the corneal epithelium can lead to the sudden onset of ocular pain, blurred vision, tearing and photophobia, typically upon awakening.
What causes this condition to appear?
There are several causes that can lead to recurrent corneal erosion. Corneal trauma is the most common cause followed by corneal dystrophies and patients with poor cornea sensation (e.g., following previous viral corneal infections, diabetics). Conditions that predispose or which can make symptoms worse include dry eyes, previous ocular surgery, ocular rosacea, Meibomian gland dysfunction, etc.
How can corneal erosion syndrome be diagnosed and how is it usually treated?
Patients usually present to the clinic with moderate to severe eye pain, photophobia and lacrimation. Ocular surface irregularity and corneal scarring lead to visual problems. On examination, areas of abrasion can be identified with loss of epithelium and fluorescein stain positive epithelial defects. Additionally, signs of predisposing conditions such as basement membrane dystrophies, previous infection / surgery, dry eyes, etc. can often be identified.
In terms of management:
- Conservative management is the first option which involves optimising the tear films with the use of frequent lubricants. Additional measures would be to optimise the health of the lid margin and ocular surface (e.g., lid care, warm compresses).
- Bandage contact lenses can be used as a short-term solution to form a barrier between the lid and the corneal epithelium to allow for corneal healing. Indefinite use of contact lenses is not recommended as it presents the additional risk of precipitating a secondary infection. Also, long term use of contact lenses from a logistics point of view is usually not very convenient for patients as it can require several visits to the clinic to replace the lenses periodically (usually every two weeks).
- Surgical techniques can be an option for treatment for cases which have failed conservative management. Examples of these are:
a. micro-puncturing the cornea
b. alcohol delamination
c. photorefractive therapeutic keratectomy.
Micro-puncture can sometimes compromise vision as it can lead to surface scarring / irregularity. Alcohol delamination and PTK are therefore the preferred surgeries.
Figure 1: Preoperative picture showing staining of area with recurrent
corneal erosions (fluorescein stain under cobalt blue filter).
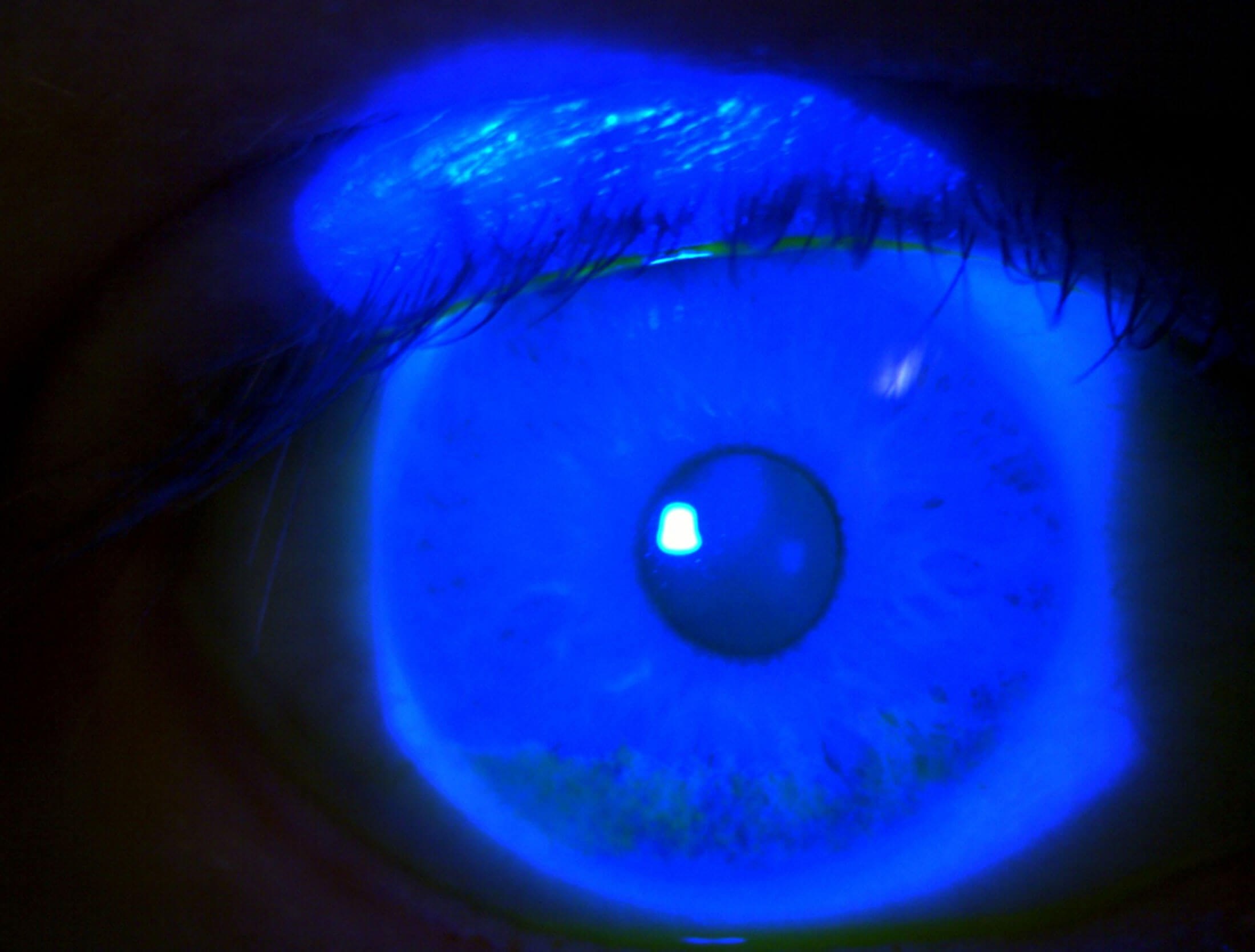
Figure 2: Postoperative picture showing lack of staining
(fluorescein stain under cobalt blue filter).
How does alcohol delamination work?
Alcohol delamination cleaves the epithelial attachment at the hemidesmosomal level leaving a smooth base behind, which is ideal in facilitating epithelial cell migration and attachment. It is usually carried out under topical anaesthesia. The cornea is treated with 18-20% alcohol for 30 seconds. Following a wash, the epithelium is completely debrided and a bandage contact lens is placed. After the epithelium has healed (usually in a week) the bandage contact lens is removed.
How does PTK work?
Phototherapeutic keratectomy is a surgical technique where the anterior cornea is treated with superficial corneal ablation. The excimer laser is used to smoothen and remove part of the bowman membrane and outer five to seven microns of stroma. Corneal epithelium then regrows with strong adhesions to the underlying stroma.
Both techniques work by removal of corneal epithelium and allow the epithelium to grow back normally. When compared, some studies have shown that when alcohol delamination was used alone, the results were similar and comparable when delamination was combined with laser. In our practice therefore alcohol delamination is considered as a first line procedure.
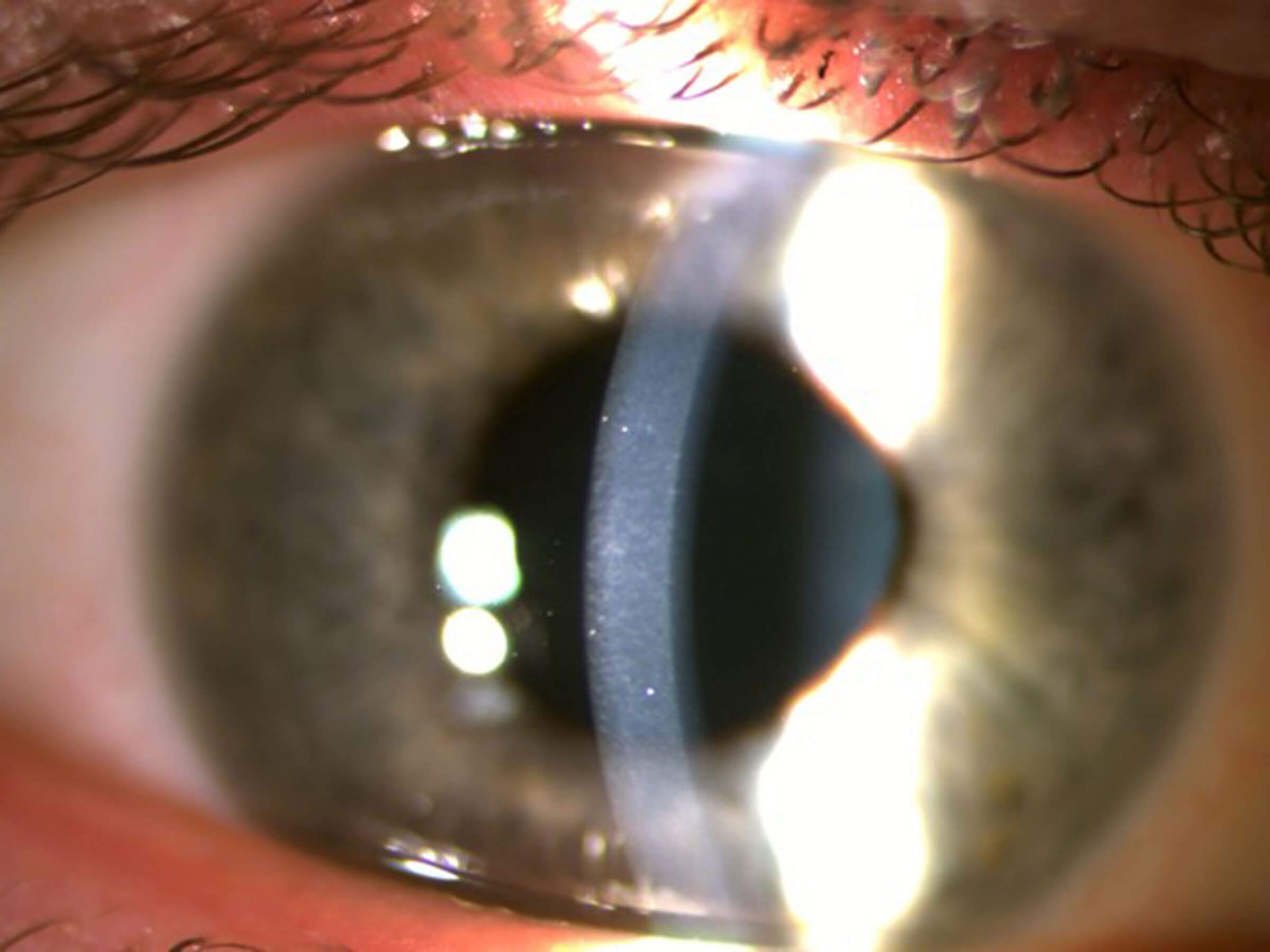
Figure 3: Preoperative slit-lamp pictures showing area of subepithelial scarring and irregularity.
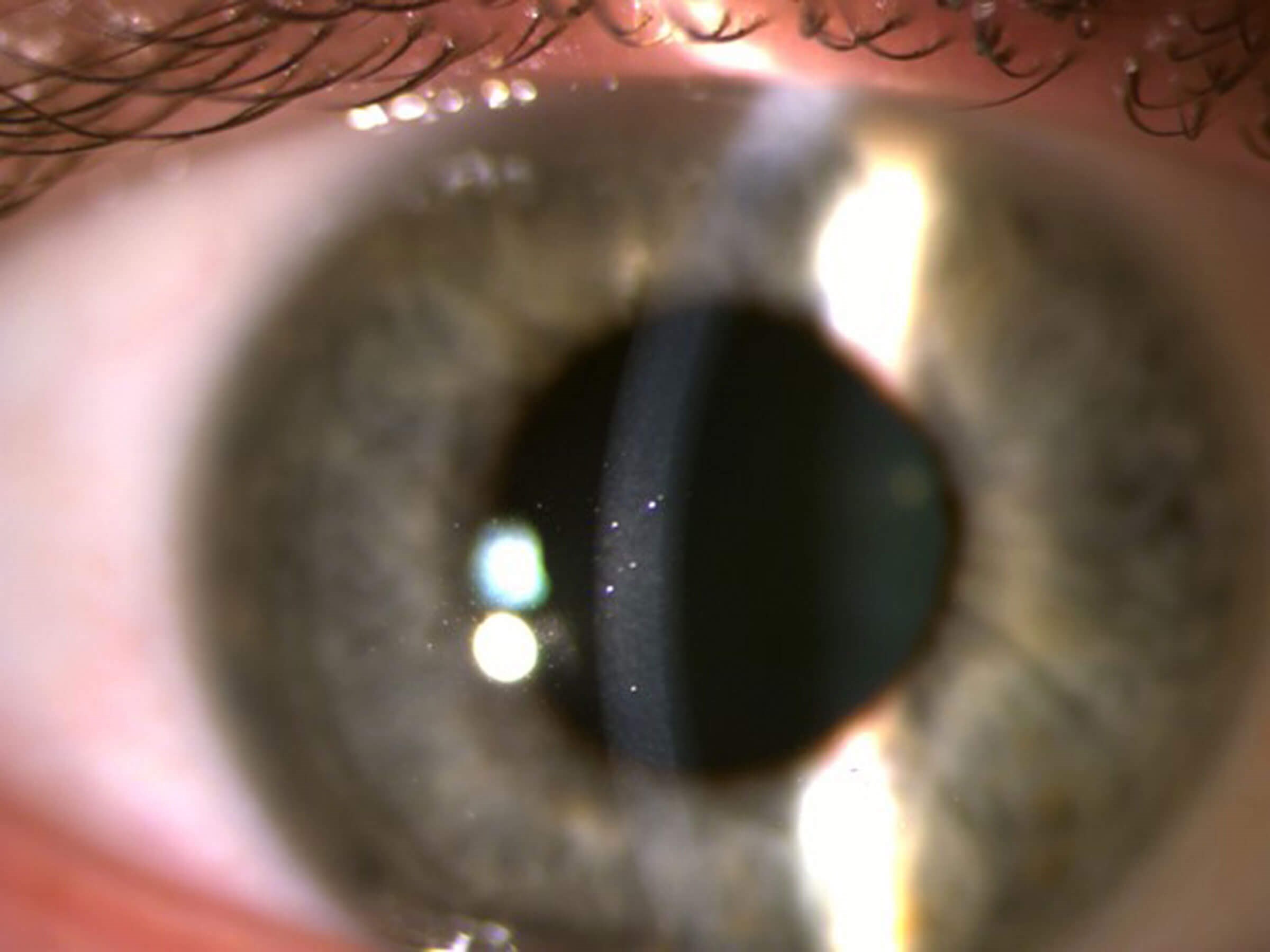
Figure 4: Postoperative slit-lamp pictures showing clear cornea.
Why would you prefer alcohol delamination over PTK as a first-line procedure?
There are several reasons why we would prefer alcohol delamination in the first instance. They are as follows:
- It is a simple and inexpensive procedure.
- It has minimal or no effect on refractive error and causes no post-operative vision change. This can be particularly relevant in asymmetric and peripheral disease. Alcohol delamination can be decentred by moving the alcohol well without any refractive problems. With PTK, decentred treatments can cause significant optical aberrations.
- There are minimal risks of post-operative scarring or haze.
- It is highly effective with a >90% success rate with no recurrence over two years in our case series.
When would you do PTK as a treatment?
PTK is used in our practice in cases of recurrence after two attempts with alcohol delamination. We would prefer PTK as first-line therapy (1) in cases which have recurred after alcohol delamination, (2) when we want to combine treatment of recurrent erosion and refractive error, and (3) if there is associated scarring involving deeper layers of the cornea to be removed by laser ablation.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME






