In 1990, the late Doctor Frank Green, a consultant ophthalmologist in Aberdeen, along with Doctor Phillip Ambler, a GP with ophthalmic training, responded to an invitation to provide ophthalmic care for Karen refugees on the northern and eastern Myanmar borders.
The refugees have been subjected to violent persecution since the 1950s, much like the recent ethnic cleansing of the Muslim Rohingya population on the western border. Thus began a very successful partnership providing ophthalmic services, mainly small incision cataract surgery (SICS), with Frank and Phillip travelling out twice a year.
After Frank retired, he volunteered at the Mae Tao Compound (MTC) in the Mae Sot district, which is dedicated to providing free healthcare to migrants and refugees in Myanmar. Supported by Karenaid, Frank worked there for over 30 weeks every year until his untimely death in 2018.

The team at SJD clinic.
Despite Frank’s absence and the COVID-19 pandemic, and largely due to Phillip’s enthusiasm, the service has continued with two ophthalmologists from Inverness who trained under Frank: Lai-Yeung Ngai and Simon Hewick. They visit both Mae Tao and the San Jai Dee (SJD) clinic near Sangkhlaburi for a fortnight twice a year. Their trips are supported by the Fiona Eye Fund, set up in memory of an ophthalmic specialist registrar from Glasgow, Fiona Dolan.
“If your unit has any relevant redundant equipment, I would be grateful if you could contact me (kateclaridge@nhs.net). Your department’s generosity will be invaluable for improving ophthalmic care to these remote populations.”
I was lucky enough to be introduced to Phillip and welcomed on a recent trip to Thailand as ‘front of house’ for their cataract service. Although the service is run on a shoestring, I was impressed by the speed with which patients were processed for SICS, largely due to the efficient pre-screening and support of Goong Sadek Nadek, an experienced Karen / Thai ophthalmic nurse, his colleagues at MTC and an army of volunteer translators.
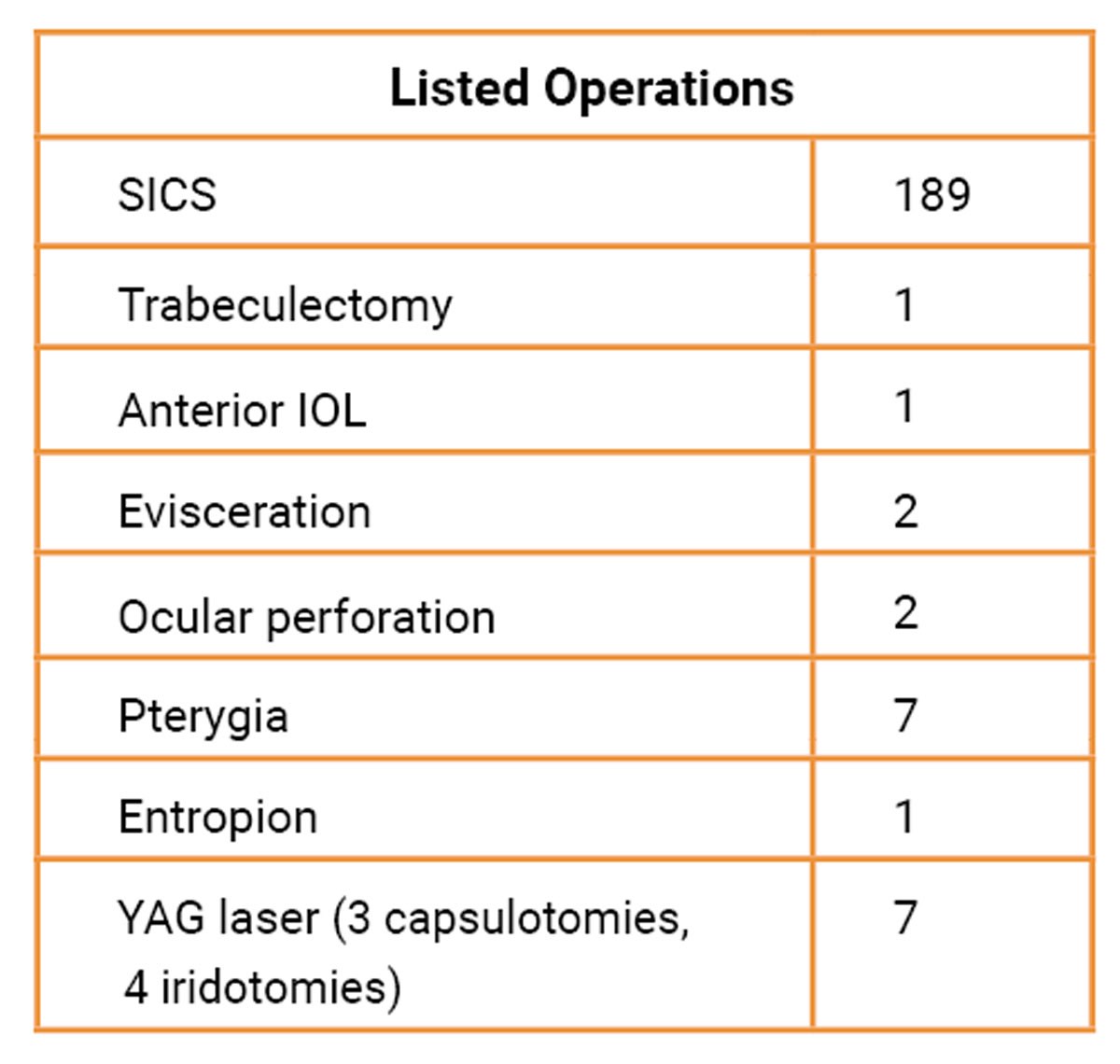
During the fortnight 263 patients were seen, of which 210 were listed for surgery (mostly SICS) and 177 procedures were completed. The others were deferred until the next trip in November.
Glaucoma is the leading cause of irreversible blindness in this population, and I was interested in its presentation and treatment. The facilities for its examination are iCare tonometry, slit-lamp examination with gonioscopy, fundoscopy and confrontation visual fields. There are no resident ophthalmologists serving these clinics and the current treatment pathway is to use timolol and acetazolamide, and to perform a YAG laser peripheral iridotomy (PI), which is only available at the SJD clinic if intraocular pressure remains high. Between the camps there is no facility for SICS or trabeculectomy, though a minority of patients access care inside Myanmar or pay for it in the Thai health system.
During the camp, there were 29 (11%) patients with definite glaucoma or having a predisposition, mostly due to primary angle closure glaucoma:
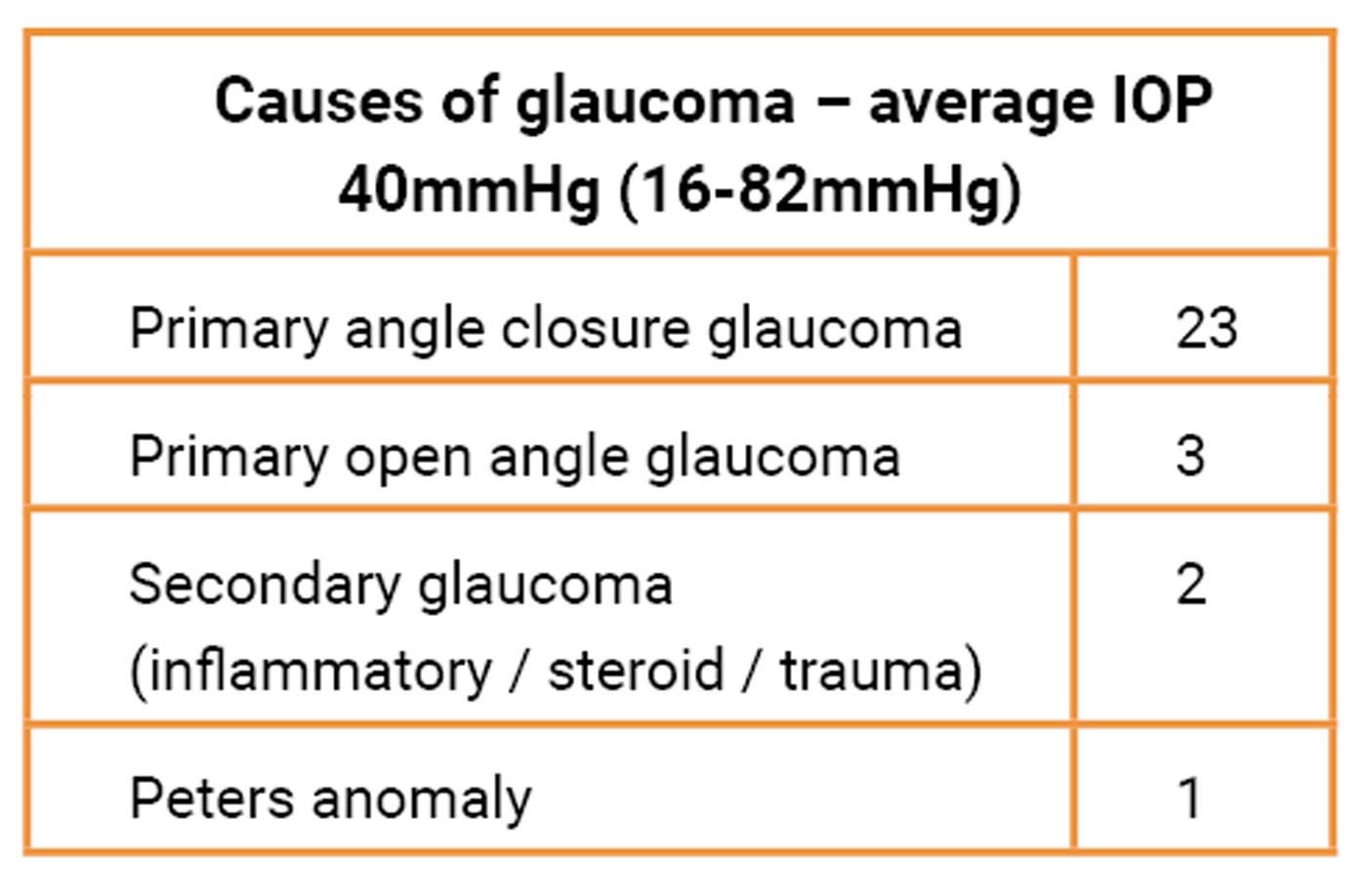
Ten eyes had no light perception, being bilateral in one patient. 17 SICS (one bilateral), one trabeculectomy and six laser PIs were performed, the long-term follow up of these patients being uncertain. It is likely the prevalence of glaucoma and angle closure disease is higher as those presenting to the camp were mainly selected for visual loss due to cataract.
There are several measures that could improve glaucoma diagnosis and management, including:
- Awareness and information for both health professionals and potential patients
- Access to visual fields and fundal imaging
- Extending the range of glaucoma medications
- Provision of laser PI and selective laser trabeculoplasty (SLT)
- Cataract surgery
- Trabeculectomy and cyclodiode laser.
Most of these will take time to purchase and establish, and I suspect there may be disused but functioning equipment in UK departments that could be transported to primary ophthalmology clinics in low- and middle-income countries. In my unit, Daybreak Medical donated our retired diode machine which is now in a Malawi clinic. Useful machines include visual fields, OCT, YAG laser for PIs, capsulotomies and possibly SLTs and cyclodiode laser.
COMMENTS ARE WELCOME





