
The steady erosion of undergraduate ophthalmology teaching, which has been acutely exacerbated by the COVID-19 crisis, has led to a lack of basic ophthalmology examining skills and knowledge amongst clinicians of other specialities. Concurrently, there has been a rise in the proportion of elderly in the population, which is contributing to the increasing prevalence of ophthalmic diseases in the general population.
Consequently, there is a risk that the lack of ophthalmology exposure at medical school will contribute to the misdiagnosis and mismanagement of ocular diseases and an overreliance on allied health specialities[1,2]. It is clear that ophthalmology teaching at medical schools must be redesigned to readdress this issue, and the disruption of the medical school curriculum caused by COVID-19 represents an excellent opportunity to do so [3].
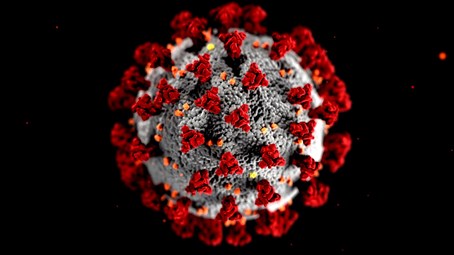
As the COVID-19 virus spread, governments soon realised that strict social distancing measures were the only way of stemming the rising infection rate. Lockdowns were imposed, with schools and universities both being shut down. Some teaching was moved online, but in general, teaching was suspended and exams were delayed or scrapped altogether. As a result, there was a reduction in the available time for medical students to shadow clinicians to further their clinical exposure. Although many medical schools asked medical students to come back early to make up for the lost clinical time, the compressed timetable on their return did not fully compensate for the lost time. This affected marginalised specialities such as ophthalmology disproportionately, where the time spent by students is already minimal.
“The steady erosion of undergraduate ophthalmology teaching, which has been acutely exacerbated by the COVID-19 crisis, has led to a distinct lack of basic ophthalmology examining skills and knowledge amongst clinicians of other specialities”
Most medical schools in the UK spend no more than two weeks of compulsory dedicated ophthalmology teaching throughout medical school, which often takes place in the final clinical years. If compressed further, it would indisputably lead to holes in essential ophthalmic knowledge. In medical schools where an ophthalmology placement was protected in length, it is quite plausible that students may have sought to use that time to brush up on skills deemed more essential or core to the medical school curriculum, thus leading to the further neglect of the ophthalmology curriculum. Given that medical students have been given the task of achieving the same competencies within a shorter period of time, we must modify ophthalmology teaching to take advantage of recently developed higher yield teaching methods, including online e-learning modules that equip medical graduates with sufficient ophthalmic skills to treat their patients. Methods for improving undergraduate ophthalmology teaching at the undergraduate level are discussed below.
Mixture of e-learning modules and recorded didactic teaching
The COVID-19 pandemic has brought e-learning, lectures over Zoom and other distance learning initiatives to the forefront of medical teaching. During the pandemic, most medical lectures, ward rounds or small group teaching groups were administered using Zoom. Later, lectures were recorded and were uploaded to virtual learning environments so that students could watch them at their convenience. These teaching methods have had a favourable response amongst medical students for specialities including ophthalmology [4]. This is because the recorded sessions or e-learning modules have allowed students to study whenever it was most convenient for them, to pause the lecture as necessary and revisit the material easily at a future date. We suggest that this change brought about by the COVID-19 pandemic should be incorporated into the future curriculum for ophthalmology given its favourable response to date.
Small group teaching Although recorded teaching and e-learning modules are highly effective, they cannot replace student-teacher interaction completely. This type of interaction is especially vital in teaching of examination techniques and their nuances. We suggest that teaching of students in small groups should continue for basic ophthalmic examination skills with an opportunity to also explore topics covered in recorded lectures and e-learning modules as well.
A specific timetable, with a logbook of conditions to see
William Osler once remarked that “To study the phenomena of disease without books is to sail an uncharted sea, while to study books without patients is not to go to sea at all.” It is imperative that students examine patients and observe their treatment in clinic. Too often, placements in all specialities are insufficiently structured, and students enter clinics without a clear understanding of what they need to observe and examine in clinic. Ophthalmology departments, in conjunction with clinical schools, should have a clear list of problems that medical students should gain competence in preparation for examining and managing patients at a primary care level.
Competency-based curriculum and a formative exam specific for ophthalmology
All the above teaching initiatives must be backed up by a competency curriculum and an exam specific to ophthalmology. Many schools incorporate assessment of ophthalmology into wider exams. As a result, students often neglect the topic in favour of higher yield specialities leading to a lack of expertise in ophthalmology. A short formative Single Best Answer(SBA) test administered at the end of an ophthalmology block mapped to the competencies they have been asked to achieve during the block may carry the necessary incentive to persuade medical students to invest the time needed to learn the essential skills of ophthalmology. Although this test will be entirely formative in that it will not contribute to final rankings or appear on a university transcript, we may use it as a method to identify students who are in further need of basic ophthalmic training. It has been shown that competency-based curriculum is both more effective and more positively received in comparison to a content-based curriculum [5].
The COVID-19 pandemic has shown that virtual teaching methods can be employed effectively, and most importantly, have been met with a positive response amongst the medical student cohort. Moving forwards from the pandemic, these teaching methods should be incorporated into a new ophthalmology curriculum to ensure that medical students graduate with the essential skills to provide basic ophthalmic care for their patients.
References
1. Stern GA. Teaching Ophthalmology to Primary Care Physicians. Arch Ophthalmol 1995;113(6):722-4.
2. Clarkson JG. Training in ophthalmology is critical for all physicians. Arch Ophthalmol 2003;121(9):1327.
3. Shih KC, Chan JC, Chen JY, Lai JS. Ophthalmic clinical skills teaching in the time of COVID‐19: A crisis and opportunity. Med Educ 2020;54(7):663-4.
4. He B, Tanya S, Sharma S. Perspectives on virtual ophthalmology education among Canadian medical students. Can J Ophthalmol Oct 2020;Epub ahead of print.
5. Succar T, McCluskey P, Grigg J. Enhancing medical student education by implementing a competency-based ophthalmology curriculum. Asia-Pacific J Ophthalmol 2017;6(1):59-63.
COMMENTS ARE WELCOME





