Virtual clinics can be used successfully in screening and management of ocular conditions such as diabetic retinopathy, retinopathy of prematurity and age-related macular degeneration. Virtual clinics should be a considered as a more clinically appropriate modality of consultation, diagnosis and monitoring of retinal disease.
Virtual clinics can be either synchronous, where patients and the physician have a consultation online in real time, or asynchronous, where the physician assesses the patient’s results including visual acuity, dilated fundus photography optical coherence tomography (OCT) scans, and colour images of the optic disc [1]. It is important to realise that these clinics involve trained health professionals such as optometrists who take patient history and measure ocular parameters.
More than two thirds of the patients in virtual glaucoma clinics did not require treatment and no difference was observed between the therapeutic outcome of patients monitored in virtual clinics or face to face (F2F) clinics [2,3]. The success of virtual clinics in glaucoma means that they can be employed for the subspeciality of medical retina and allow patients to be assessed accordingly based on their clinical need, reducing the burden on hospital eye services. This would prove to be both a cost-effective and operationally efficient solution to the capacity issues currently faced by the NHS and has already shown to improve the patient’s healthcare experience [4].
Results and discussion
Diabetic retinopathy (DR) is the most common presentation at clinics, with the prevalence of diabetes estimated to increase by 1.0-4.1% annually in the UK [5]. Forty-three million cases of sight-threatening DR is expected by 2035, which is almost double that of 2012 [6]. Since 2003 in the UK, diabetic retinopathy screening services (DRSS) have effectively reduced visual loss from diabetic eye disease. This has meant that in the working population in England, DR is no longer the foremost causative factor of blindness [7] However, trends in the last five years have shown that as more people are screened, more DR is detected, and this has reduced the threshold for referral with an increase of 30% in eye clinic appointments [8].
Macula oedema from retinal vein occlusion and DR in the elderly and in diabetic patients are important causes of visual loss [9]. Due to the sight-threatening consequences of macula oedema, multiple hospital visits are required for intravitreal anti-vascular endothelial growth factor injections (anti-VEGF) [10]. This instigates the imbalance between supply and demand which is also becoming a global issue [11]. This can be overcome by increasing efficiency of clinics, e.g. by increasing the number of virtual clinics or by redistributing jobs to other members of the medical team. The Royal College of Ophthalmologists found that approximately 20 patients every month experience significant deterioration to their vision as a result of waiting for their appointment [1]. If virtual clinics can select patients requiring urgent F2F appointments, avoidable vision loss can be prevented and consequently improve the quality of life of these individuals.
By 2035, the elderly population is projected to be 2.5 times greater. This estimates age-related macular degeneration (AMD) to rise by 60% and those seeking clinical care will also substantially increase [12]. Virtual clinics provide an opportunity to widen access to care for this population, mitigating distance barriers. With the current climate where social distancing has been inflicted upon us, virtual clinics lower the susceptibility to COVID-19 by preventing overcrowding in clinics and allow for ongoing care to take place. This benefits clinically vulnerable people who are unable to leave their homes. A study showed that virtual clinics reduced patient waiting times by 25% and physician time by 50% [13]. This allows high-risk cases to be assessed by experienced consultants in a timely fashion and reduces the incidence of sight-threatening consequences. Continuous monitoring of pathology in low-risk cases can occur more consistently as fundus photographs and OCT scans can be performed in the community. This can improve compliance with follow-up clinic appointments.
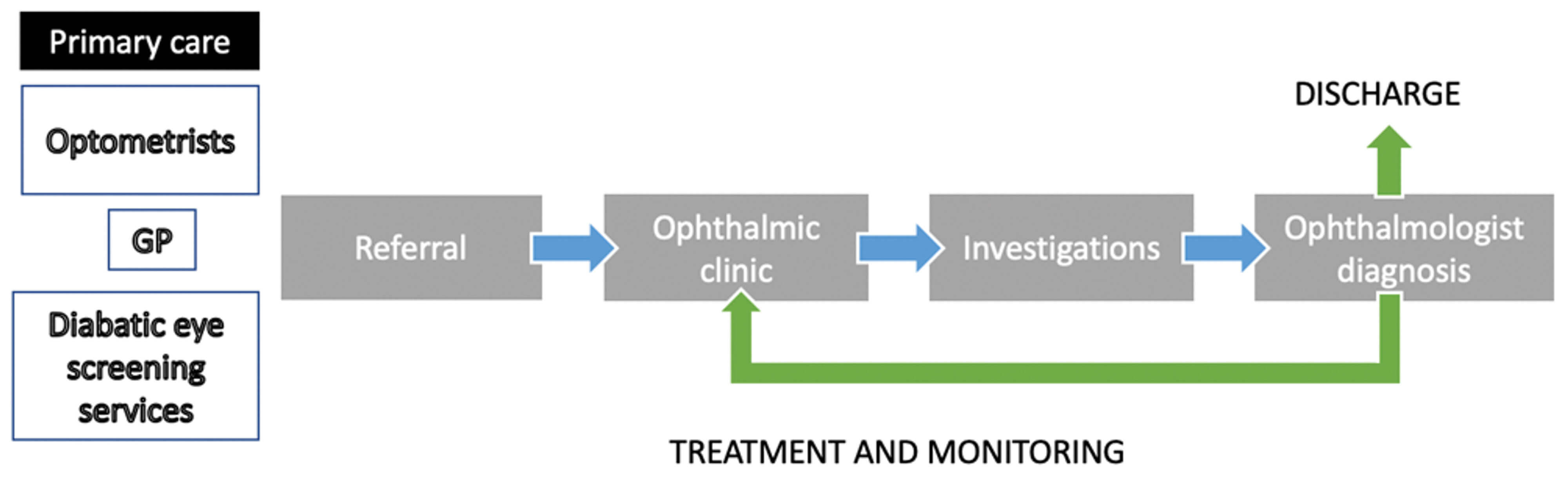
Figure 1: Traditional pathway for retinal eye disease.
This diagram shows the traditional referral pathway for retinal eye disease.
All referred patients from primary care are seen in
face to face (F2F) ophthalmic clinics and investigated.
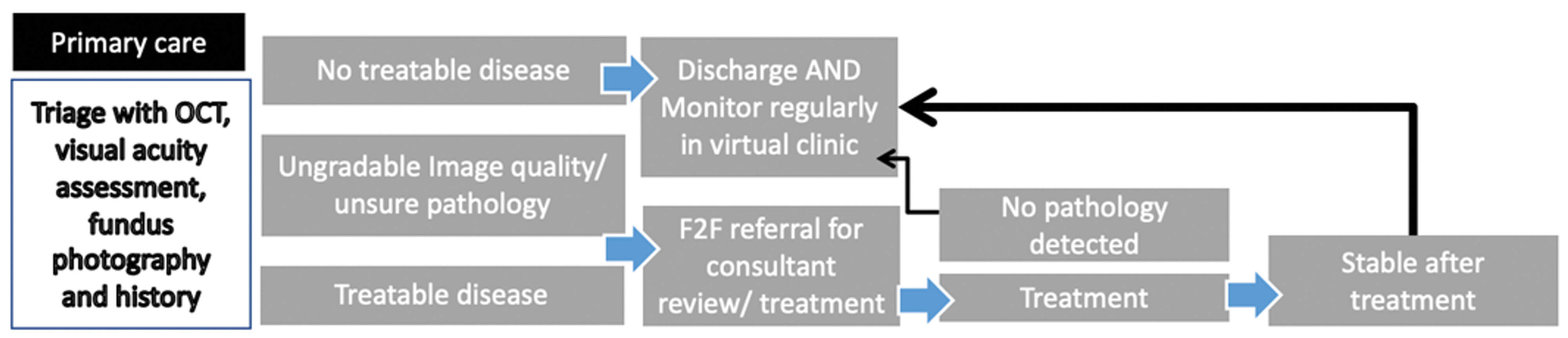
Figure 2: Virtual clinic pathway for retinal eye disease.
This diagram shows the referral pathway with virtual clinics for retinal eye disease.
The aim is to increase efficiency of clinics by triaging patients in primary care
and providing focused treatment according to clinical need.
A study of 1729 patients attending the virtual clinic at Moorfield’s eye hospital found that only 0.7% of patients were referred to the F2FC, mainly due to poor image quality as a result of poor technique or cataract obscuring the view [1]. If a disease was seen as potentially treatable, these individuals were also referred for F2FC (20.2%) [1]. This is supported by a retrospective study of 610 new patients who were seen in the medical retina virtual clinic between April 2016 and May 2018; 27.8% of these patients were referred to F2FC for treatment and this was the main reason for referral [14]. Image quality was inadequate in only 0.3% of cases. Overall, only 1/4 of patients were referred to F2FC and this shows that virtual clinics have a substantial role in filtering patients according to clinical need. Again, these two studies revealed a short follow-up time to appointments of eight and 12 days respectively and increased capacity in the F2F medical retina clinics.
A wide array of retinal pathologies can be followed-up and reviewed remotely using OCT, OCT angiography and colour fundus photography. Conventionally, specialist eye clinic appointments are used to assess oedema in diabetic maculopathy. The Cochrane review has investigated the safety and effectiveness of virtual clinics. OCT proves to have a greater level of accuracy than slit-lamp examination in assessing macula oedema [15,16]. The conclusion from the study was that OCT should have a formal role in the diagnosis of diabetic macular oedema [15]. A study involving 51 new referrals over a three-month period from the National Diabetic Eye Screening programme (DESP) used widefield Clarus imaging and macular OCT and slit-lamp clinical examination and macular OCT to compare how DR was graded between virtual clinics and F2F clinics [17]. In this study, 2/3 of DESP referrals were managed effectively in virtual clinics using widefield Clarus and macular OCT imaging [17]. Clarus widefield fundus camera provides better image quality and in true colour, making it a useful tool for assessing the fundus in detail. It may be useful to lower the threshold for referral to F2F clinics if signs of serious retinal pathology are found in virtual clinics.
It would be more efficient if DRSS or eye hospitals triage referrals with OCT imaging prior to making referrals to F2F clinics. This would enable treatable retinopathy to be seen in secondary care only and be a cost-effective solution.
The safety and efficiency of virtual clinics can be assessed using factors such as the mean time to follow-up, number of F2F referrals and consistency in optical measurements. Another retrospective study of 728 patients at Moorfields Eye Hospital between November 2016 and July 2018 showed a decrease in the time from referral to appointment by eight days and this allows low risk referrals to access virtual clinics promptly as a first-line option [2]. There was no decline in mean visual acuity or mean DR severity grades between virtual appointments [2]. The consistency in the results, along with reduced urgent referral rates, support the safety of virtual clinics. Supporting this, one study showed that across five primary care clinics, there was >90% agreement between the findings from a virtual clinic and F2F clinic [13]. This demonstrates that virtual clinics do not compromise patient safety and are able to provide accurate results. Any uncertainties, from poor imaging or suspicion of high risk, are promptly referred for F2F consultations.
It is important to consider the quality of care and patient acceptance in virtual clinics. A retrospective cohort study of 12,563 diabetic patients referred by the DESP to either a virtual or an F2F appointment at the Moorfields Eye Hospital between January 2015 and December 2018 showed that attendance rate of virtual (72%) and F2F consultations (68%) were similar [8]. Moreover, mean time to referral to their first hospital appointment and discharge was 14 days less in virtual clinics (66.9 days) when compared to F2F clinics (80.9 days) [8]. No statistically significant difference was observed in the mean time to treatment for those requiring intravitreal therapy for maculopathy [8]. This data is reassuring, as this indicates that patients are accepting of virtual clinics and shows no compromise to patients’ access to treatment or quality of care.
The UK Department of Health encourages non-medical healthcare professionals to take up OCT and widefield devices training in an attempt to improve optic media processing and reduce poor quality images. Moreover, a study involving 300 patients over a seven-month observation period found ophthalmologists and photographers 100% in agreement on the proposed management plan with no reports of safety concerns [18]. The clinic capacity also increased by 24% [18]. Following a virtual assessment by non-medical healthcare professionals, patients can be informed via letter about follow‑ups / treatment. This allows more time for the patients to think and make an informed decision on their treatment options. If they are referred for a F2F appointment, any questions they may have acquired after the virtual clinic can be addressed here.
However, not all retinal pathology would be suitable for virtual clinics. Severe non-proliferative DR or recently treated proliferative DR cannot be assessed in virtual clinics as angle measurements cannot be taken [1]. Although photic maculopathy can be identified from images, confirmation is dependent upon questioning the patient directly [17]. To overcome this, virtual assessment should be used along with phone consultations, this would enable the history to be taken simultaneously. Other problems such as a hazy fundus view due to cataracts could limit the success of virtual clinics. Pathologies causing reduced vision may not always be revealed by retinal imaging, however, improved anterior segment and optic disc imaging may aid virtual clinics in this [17]. Patients with physical disabilities may find it difficult to position themselves correctly to obtain fundus pictures and this may make virtual clinics inappropriate for this sub cohort.
Future work
Virtual clinics may feel impersonal due to the lack of patient rapport with the medical team and understanding patient’s acceptance and satisfaction in virtual clinics is important. Although patient acceptability has been reported to be similar in virtual and F2F glaucoma clinics, a study needs to be performed in virtual medical retina to confirm this.
Future larger prospective studies with longer periods of follow-up can help assess the safety and efficacy of virtual clinics by comparing it with current clinical standards. Regular audits and feedback are required to make sure quality and high care standards are met. Prospective studies are needed to assess whether patients with high-risk retinal disease may be eligible for virtual assessment and to alter current triage guidelines.
Conclusion
Virtual clinics appear to be the way forward for the diagnosis and management of retinal diseases as they are able to act as first-line rapid access clinics for low-risk referral. Together with optimising the use of existing resources, virtual clinics reduce the burden on hospital eye services. Existing members of the healthcare team can be trained without compromising quality of clinical standards. Mixed pathology clinics allow increased capacity in pressurised medical retina. Artificial intelligence and algorithms such as Deep Learning on OCT retinal scans can be integrated to promote upskilling the workforce and provision of resources [2,19]. Promoting shared care of patients in virtual clinic settings between ophthalmologists, optometrists, nurses and optical photographers would help reduce pressure and sight-threatening cases are less likely to be missed.
TAKE HOME MESSAGE
-
Virtual clinics can increase capacity, time to first appointment and time to discharge.
-
Low risk retinal pathology can be triaged in the community using OCT imaging, preventing sight-threatening cases from being missed.
-
Existing members of the healthcare team can be trained. Ophthalmologists and photographers have high rates of agreement in the proposed management plan.
-
Attendance rates are similar for F2F and virtual clinics and this might improve compliance.
-
Virtual clinics are a good alternative during a pandemic and for frail patients.
-
Shared care and continuous monitoring will lead to better outcomes with fewer patient lost to follow-up.
References
1. Kortuem K, Fasler K, Charnley A, et al. Implementation of medical retina virtual clinics in a tertiary eye care referral centre. Brit J Ophthalmol 2018;02(10):1391-5.
2. Kern C, Kortuem K, Hamilton R, et al. Clinical Outcomes of a Hospital-Based Teleophthalmology Service. Ophthalmol Retina 2019;3(5):422-8.
3. Trikha S, Macgregor C, Jeffery M, Kirwan J. The Portsmouth-based glaucoma refinement scheme: a role for virtual clinics in the future? Eye 2012;26(10):1288-94.
4. Kanji A, Jojo V, Schmermer S, et al. Managing patients with early diabetic maculopathy via virtual SD-OCT clinics. Diabetic Eye J 2015;4:34-8.
5. Shaw J, Sicree R, Zimmet P. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010;87(1):4-14.
6. Yau JW, Rogers SL, Kawasaki R, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care 2012;35:556-64.
7. Olafsdóttir E, Stefánsson E. Biennial eye screening in patients with diabetes without retinopathy: 10-year experience. Br J Ophthalmol 2007;91:1599-601.
8. Faes L, Fu D, Huemer J, et al. A virtual-clinic pathway for patients referred from a national diabetes eye screening programme reduces service demands whilst maintaining quality of care. Eye October 2020; Open Access.
9. Kobrin Klein B. Overview of Epidemiologic Studies of Diabetic Retinopathy. Ophthalmic Epidemiol 2007;14(4):179-83.
10. Stewart M. Treatment of diabetic retinopathy: Recent advances and unresolved challenges. World J Diabetes 2016;7(16):333.
11. Resnikoff S, Felch W, Gauthier T, Spivey B. 2012. The number of ophthalmologists in practice and training worldwide: a growing gap despite more than 200 000 practitioners. Brit J Ophthalmol 2012;96(6);783-7.
12. Age-Related Macular Degeneration and Diabetic Retinopathy. London: The Royal College of Ophthalmologists; 2015. The Way Forward. Options to Help Meet Demand for the Current and Future Care of Patients with Eye Disease:
https://www.rcophth.ac.uk/wp-content/
uploads/2015/10/RCOphth-The-Way
-Forward-AMD-300117.pdf.
Last accessed June 2021.
13. Maa A, Wojciechowski B, Hunt K, et al. Early Experience with Technology-Based Eye Care Services (TECS). Ophthalmology 2017;124(4):539-46.
14. Lee J, Manjunath V, Talks S. Expanding the role of medical retina virtual clinics using multimodal ultra-widefield and optical coherence tomography imaging. Clin Ophthalmol 2018;12:2337-45.
15. Virgili G, Menchini F, Dimastrogiovanni AF, et al. Optical coherence tomography versus stereoscopic fundus photography or biomicroscopy for diagnosing diabetic macular edema: a systematic review. Invest Ophthalmol Vis Sci 2007;48(11):4963-73.
16. Virgili G, Menchini F, Casazza G, et al. Optical coherence tomography (OCT) for detection of macular oedema in patients with diabetic retinopathy. Cochrane Database Syst Rev 2015;1:CD008081.
17. Lim W, Grimaldi G, Nicholson L, et al. Widefield imaging with Clarus fundus camera vs slit lamp fundus examination in assessing patients referred from the National Health Service diabetic retinopathy screening programme. Eye 2020;35(1):299-306.
18. El-Khayat A. Ophthalmic photographer virtual clinics in medical retina. Int J Ophthalmol 2020;13(4):677-80.
19. De Fauw J, Ledsam J, Romera-Paredes B, et al. Clinically applicable deep learning for diagnosis and referral in retinal disease. Nature Medicine 2018;24(9):1342-50.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME






