The authors provide a case of cyanoacrylate glue causing a thermal burn on the eyelid and explain how this type of burn should be managed.
The use of false lashes as well as the techniques used to apply them come with an increased risk of exposing the eye and the eyelids to harmful substances. We report the first known case where the glue used to apply false eyelashes caused lid burn injuries and, consequently, a significantly inflamed and painful eyelid.
Case report
We report a case of a 17-year-old female who presented to eye casualty with a significantly painful and red eyelid 24 hours after having false eyelashes applied. False eyelashes are widely available over the counter, online or from a beautician. There are two main types of false lashes: one comes as a strip and usually lasts for a day, while the other involves individual lashes being applied and usually lasts for around three weeks on average. This patient had used the daily false lashes previously but this time she opted to have the individual lashes applied by a beautician.

Figure 1: A right erythematous and oedematous upper lid with two areas of superficial skin loss secondary to cyanoacrylate-based glue used to apply false eyelashes.
At presentation, the right upper lid was significantly inflamed with two areas of superficial skin loss above the eyelashes (Figure 1). On further examination, there were distinct areas of epithelial defect on the right upper lid measuring around 2mm in diameter, which only involved the epidermis. Her visual acuity was 6/6 and ocular examination was unremarkable, with no sign of conjunctival or corneal involvement. The left eye and eyelids were normal.
The patient and her mother were initially concerned about an allergic reaction to the glue and questioned whether the eyelashes should be removed. Careful examination revealed the eyelid defects were above the eyelashes and the base of the eyelashes were not inflamed, which made an allergic reaction to the glue less likely. Furthermore, the left eye, which had also had new eyelashes, remained quiet. The patient also informed us that patch testing with the glue on her forearm was performed at least 24 hours prior to having the eyelashes applied and did not suggest any allergy to the glue.
Given the history of foreign material near the eye, the pH of the tear film was also tested which was neutral. The lid margin, lash line (including the false lashes) were continuous. The defects only involved the superficial layer of the eyelid and there was no blistering. The areas of defect on the eyelid were irrigated with basic salt solution after instilling topical anaesthesia. Oral co-amoxiclav 500/125mg three times a day along with chloramphenicol ointment four times a day was given to prevent secondary infection.
Due to the epithelial defects on the eyelid skin and significant periorbital erythema, lubricating eye drops were also provided for symptomatic relief. No dressings were used. The patient was reviewed three days later, by which time the inflammation had settled and she was asymptomatic. She was very happy with the outcome and especially thrilled that she did not need to have her new lashes removed.
Discussion
The predominant component of eyelash glue is ethyl cyanoacrylate. Cyanoacrylate is an acrylic resin that sets rapidly once coming into contact with moisture [1]. Cyanoacrylates are strong adhesives used for a variety of medical, industrial and cosmetic applications [2]. Although used widely, there are known risks associated with such products. Dermabond® (2-octyl-cyanoacrylate; Ethicon UK) a skin adhesive for example, has been shown to cause contact dermatitis [3]. Cyanoacrylates used specifically as eyelash glue have also been shown to cause bilateral eyelid erythema and swelling due to an allergic reaction [4,5].
The main differentials of this case include chemical burn, contact dermatitis, an allergic reaction to cyanoacrylate glue and thermal burn injury. As described in the case report, there are a few reasons as to why an allergic reaction is unlikely. A negative patch test, a lack of inflammation around the base of the false lashes in the right eye and a quiet left eyelid put an allergic reaction lower in our list of differential diagnoses. Both contact dermatitis and burns can cause erythema, swelling and blistering. However, contact dermatitis is nearly always itchy, which is not the main symptom of our patient.
It is important to clarify that the type of burn caused by cyanoacrylate glue is a thermal burn and not a chemical burn [6]. By definition, a chemical burn of the skin occurs as a result of corrosive substances such as strong acids or alkalis being in contact with the skin. A thermal burn, on the other hand, occurs due to an external heat source, which raises the temperature of the skin, causing cell death. As cyanoacrylate sets after contacting moisture, there is an exothermic reaction which can lead to this rise in temperature [7]. The depth of burn depends on the temperature and duration of exposure [8]. A study on the relationship between time and exposure by Mortiz and Henriques, suggests that exposure for more than one second at 60°C can cause partial-thickness burns [9]. According to Kelemen et al. high temperatures of 68°C can be produced by the exothermic reaction of cyanoacrylate setting, which is more than enough to cause partial-thickness skin burns [10]. As far as we are aware, this is the first reported case in literature in which a patient has presented with unilateral lid swelling with obvious lid burns from the use of a cyanoacrylate glue.
Factors that can increase the risk of cyanoacrylate glue associated burns include larger volumes (which liberate more heat as well as affect a larger area) and lower viscosity of the glue (which increases the distribution of the glue, again resulting in a larger area being affected) [6]. Cotton also seems to act as a catalyst in this exothermic reaction. The β-linked glucose units of cotton provide a large number of hydroxyl groups that is required for the polymerisation of cyanoacrylate. This results in the same amount of thermal energy being liberated but over a shorter period of time. This intense accumulation of heat thus leads to thermal injuries, therefore an important material to avoid when there is a history of the use of cyanoacrylate glue.
Artificial nail glue, which is also cyanoacrylate based, has been known to cause skin burns. A case-series by Coles et al. described four cases of thermal burns caused by cyanoacrylate-based nail adhesives [1]. A further report by Bélanger et al. described a case where a five-month old girl required hospitalisation for treatment and supervision after accidental spillage of nail adhesives [11]. Some patients have also required surgical debridement and skin graft reconstruction following burns injuries from cyanoacrylate nail glue [6]. Management therefore depends on the severity and location of the burn and may require input from the plastics / burns unit. Burns from cyanoacrylate glues around the eye should be managed as any periocular burn.
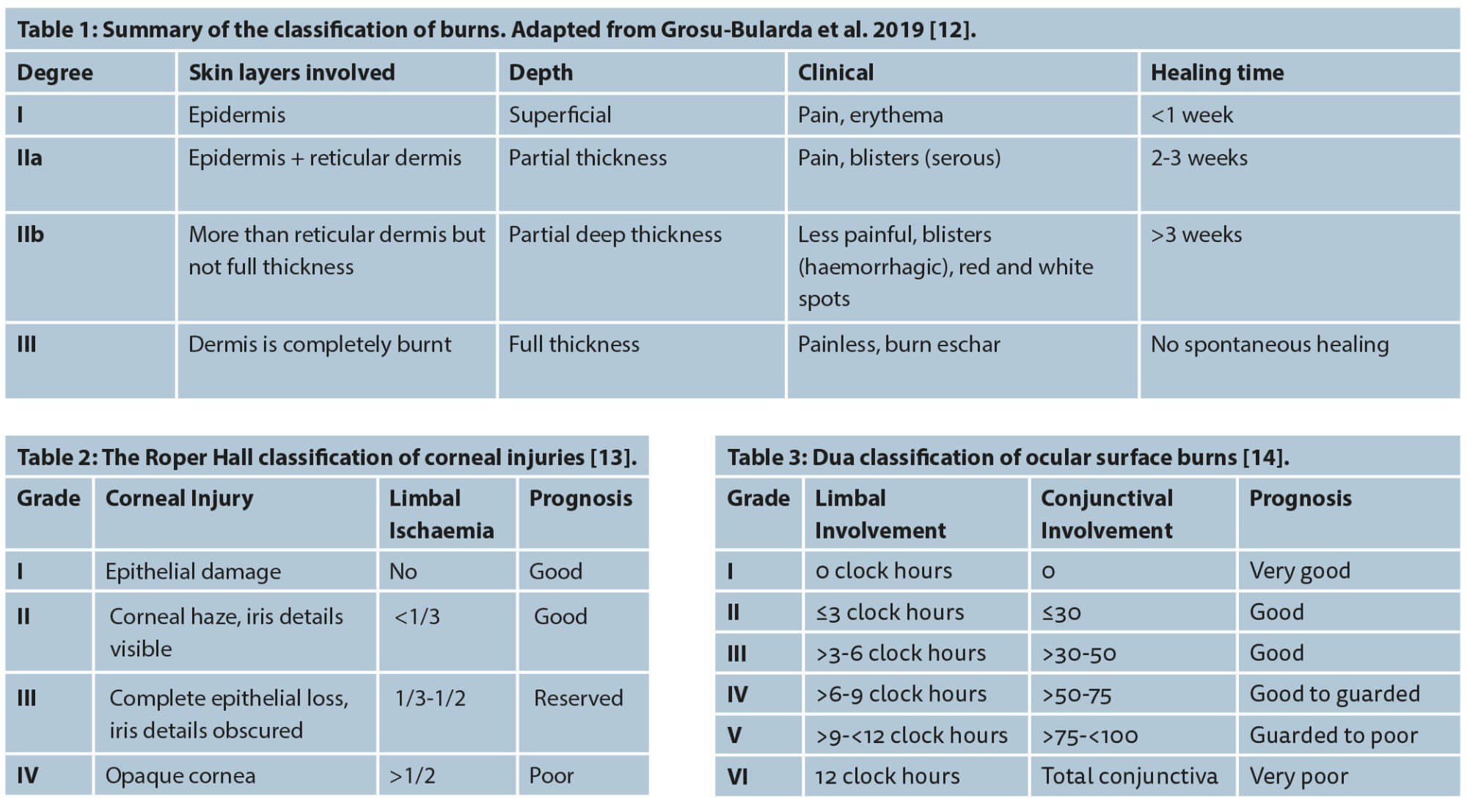
Burns are classified based on how deep the skin is affected (Table 1). Ocular surface involvement is graded by the Roper Hall Classification (Table 2) [13] or the Dua classification (Table 3) [14]. In the acute phase of a burn injury, the patient should be stabilised as per the advanced life support guidelines with emphasis on stabilisation of vital functions and fluid resuscitation [12]. The Parkland formula is used to calculate the amount of fluid required in burns patients in 24 hours: 4ml Hartmann’s solution x body weight (kg) x total burn surface area (%).
Half of this calculated volume is administered in the first eight hours and the other half given over the following 16 hours.
Management of periocular burns is determined by the severity of the periocular burn and whether the eye is involved. In order of importance, the aims of managing periorbital burns are to preserve vision, prevent secondary complications and restore an acceptable aesthetic outcome [15].
Specifically, for periorbital burns, wounds should be washed and foreign bodies removed. It is imperative that the eyelids are opened and the eye is irrigated thoroughly too with saline solution and any foreign bodies removed [12]. The use of lubricating ointment, topical antibiotics, temporary tarsorrhaphy, conjunctival flaps, amniotic grafts and skin grafting may be required to protect the ocular surface [15]. Periorbital burns involving the eyelids and eyelashes are more likely to have associated ocular surface injuries [16]. Protective measures should be taken to protect the eye even if it is not involved in the initial injury. Loss of skin or skin contracture may lead to exposure keratopathy during a patient’s admission, and so it is important that the ophthalmologist continues to monitor patients with periocular burns daily. Long-term follow-up duration and frequency depend on the severity of the injury, ocular involvement and the risk of long-term complications. Burns following electrocution, for example, can have long-term ophthalmic sequelae including cataract formation within a year from the injury and more rarely chorioretinal atrophy [16]. In such cases patients should be reviewed every three months once discharged from hospital [12].
“Loss of skin or skin contracture may lead to exposure keratopathy during a patient’s admission, and so it is important that the ophthalmologist continues to monitor patients with periocular burns daily”
In this case, the burn was classified as a first degree burn with no ocular surface involvement. The wound was washed out and any remnant glue was removed, care was taken to not use any cotton buds or cotton dressings. Lubricating and antibacterial ointment was used to protect the ocular surface and there was a good clinical outcome.
In summary, cyanoacrylate glue associated thermal burns are rare but can be very severe. Risk factors of thermal burns associated with cyanoacrylate glue are large volume of glue used, low viscosity of the glue and the presence of cotton. Beauticians and clinicians should be aware of these risk factors. An inflamed eyelid after application of false eyelashes is usually thought to be the result of an allergic reaction. However, this case exemplifies that thermal burns could also be a potential cause and clinicians should look for evidence of this on examination.
References
1. Coles C, Javed MU, Hemington Gorse S, Nguyen D. Paediatric burns secondary to nail adhesives: a case series. Burns Trauma 2016;4(1):17.
2. Cook KA, White AA, Shaw DW. Patch Testing Ingredients of Dermabond and Other Cyanoacrylate-Containing Adhesives. Dermatitis 2019;30(5):314-22.
3. Sato M, Inomata N, Aihara M. A case of contact dermatitis syndrome caused by Dermabond®, followed by contact dermatitis caused by false eyelash glue and Aron Alpha® glue: possibility of cross-reactions among cyanoacrylates. Contact Dermatitis 2017;77(6):414-5.
4. Mimura T. Bilateral eyelid erythema associated with false eyelash glue. Cutan Ocul Toxicol 2013;32(1):89-90.
5. Shanmugam S, Wilkinson M. Allergic contact dermatitis caused by a cyanoacrylate-containing false eyelash glue. Contact Dermatitis 2012;67(5):309-10.
6. Eyth CP, Echlin K, Jones I. Cyanoacrylate Burn Injuries: Two Unusual Cases and a Review of the Literature. Wounds 2016;28(12):e53-9.
7. Moossavi M, Scher RK. Nail care products. Clin Dermatol 2001;19(4):445-8.
8. Malhotra R, Sheikh I, Dheansa B. The management of eyelid burns. Surv Ophthalmol 2019;54(3):356-71.
9. Moritz AR, Henriques FC. Studies of Thermal Injury: II. The Relative Importance of Time and Surface Temperature in the Causation of Cutaneous Burns. Am J Pathol 1947;23(5):695-720.
10. Kelemen N, Karagergou E, Jones SL, Morritt AN. Full thickness burns caused by cyanoacrylate nail glue: A case series. Burns 2016;42(4):e51-4.
11. Bélanger RE, Marcotte ME, Bégin F. Burns and beauty nails. Paediatr Child Health 2013;18(3):125-6.
12. Grosu-Bularda A, Andrei MC, Mladin AD, et al. Periorbital lesions in severely burned patients. Rom J Ophthalmol 2019;63(1):38-55.
13. Roper-Hall MJ. Thermal and chemical burns. Trans Ophthalmol Soc UK 1965;85:631-3.
14. Dua HS, King AJ, Joseph A. A new classification of ocular surface burns. Brit J Ophthalmol 2001;85:1379-83.
15. Fitzgerald O’Connor E, Frew Q, Din A, et al. Periorbital burns – a 6 year review of management and outcome. Burns 2015;41(3):616-23.
16. Capek KD, Culnan DM, Merkley K, et al: Burn Injuries of the Eye. In Total Burn Care. Fifth Edition. Herndon DN (Ed). Elsevier; 2018:435-44.
COMMENTS ARE WELCOME