History
A 58-year-old female patient was referred with a 2-year history, gradually enlarging, painless left upper lid lump. There was no bleeding or ulceration. She had no other eye symptoms and no other skin lesions.
- Her past medical history included: hypertension and gastro-oesophageal reflux disease, which were controlled by medication.
- On examination: vision in both eyes was 6/9 aided; there was a left upper lid non-mobile, non-tender nodular lesion on the lid margin with madarosis. Anterior segments and fundoscopy were otherwise normal.
- A left eyelid shave excision biopsy was performed and sent for ophthalmic pathology assessment.
- Macroscopic examination showed a lash-bearing skin measuring 5 x 5 x 4mm with a nodule measuring 3mm in diameter and 1mm from the peripheral margins
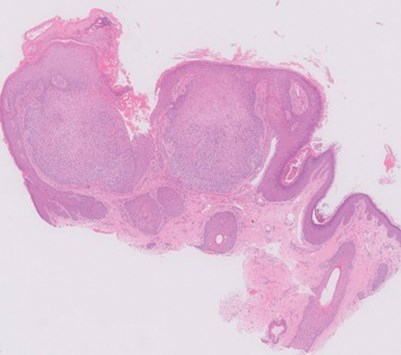
Figure 1a.
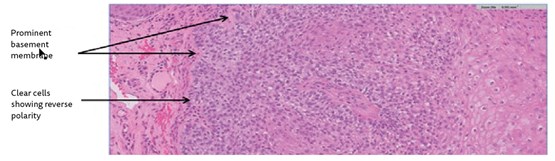
Figure 1b.
Questions
- Figures 1a and 1b show representative H&E sections of the lesion. How can this be described?
- What are the differential diagnoses?
- What is the most likely diagnosis and what further stains may help?
Answers
1. Figure 1a (H&E x2) shows a bulbous, basaloid squamoproliferative tumour in continuity with the epidermis, with hyperkeratosis, peripheral palisading and some clear cells peripherally showing reverse polarity (Figure 1b; H&E x20). There is subtle stromal clefting. The tumour is surrounded by a prominent basement membrane (Figure 1b). There is no evidence of dysplasia or malignancy.
2. Differentials include: basal cell carcinoma (BCC: abnormal mitoses, artefactual clefting with mucin within the spaces); squamous cell carcinoma (SCC: cellular atypia, abnormal mitoses, invasive borders, necrosis); inverted follicular keratosis (small basaloid cells and squamous eddies), viral wart (prominent papillomatosis, with hyperkeratosis and spires of parakeratosis, prominent granular cell layer).
3. The appearances are those of a TRICHILEMMOMA/TRICHOLEMMOMA, with complete excision. No further stains were necessary in this case as the histomorphological features were characteristic. However, the similar outline, basaloid features with stromal clefting and peripheral palisading may be confused with a BCC. Immunohistochemistry can help. BCC is strongly BerEp4 immunopositive and CD34 negative, whereas a trichilemmoma is CD34+ and BerEp4-.
Desmoplastic trichilemmomas with desmoplasia within the tumour and squamous morules can mimic a SCC (CD34- but would demonstrate malignant histomorphological features outlined above).
Trichilemmomas are benign follicular tumours (derived from the outer root sheath of the hair follicle), which typically present in the head and neck areas in middle-aged adults with no gender predilection. Complete excision is curative. Multiple trichilemmomas may be a manifestation of Cowden syndrome, an autosomal dominant genodermatoses associated with mutation in the PTEN tumour suppressor gene. The syndrome is associated with multiple trichilemmomas, mucosal papillomas, various hamartomas and may present an increased risk of carcinomas (thyroid, breast and gastrointestinal tract).
COMMENTS ARE WELCOME





