History
-
A 62-year-old female patient was referred for rapid growth of a left periorbital soft tissue lesion with proptosis.
-
Her past medical history included: hypertension, hyperlipidaemia and bipolar disorder.
-
On examination: vision in the affected eye was hand movements, right eye was 6/9 aided; there was a palpable left periorbital mass; marked anterolateral proptosis and fixed globe with no extraocular movements.
-
A left lateral canthotomy with upper and lower lid cantholysis was performed and an incisional biopsy of the lesion was sent for ophthalmic pathology assessment.
-
Macroscopic examination revealed a gelatinous pale mass measuring 12x8x6mm.
-
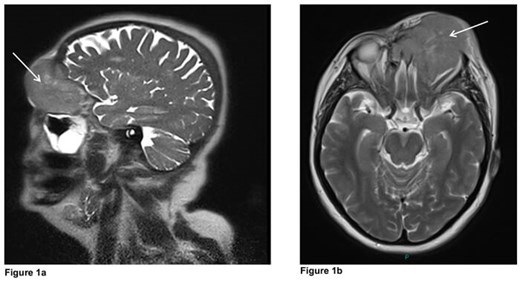
In the meantime, MRI head and orbits with contrast (Figures 1a and b) showed a left orbital tumour (white arrows) measuring 7x5.4x6cm displacing the globe anterolaterally and extending to the paranasal sinuses, left nasal cavity with bifrontal extradural extension.
Questions
-
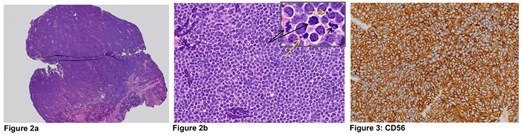
Figures 2a and b show a representative H&E section of the lesion. How can this be described?
-
What immunohistochemical stains would help?
-
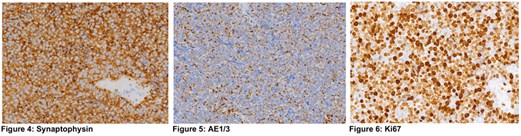
Figures 3-6 demonstrate positive immunostaining for select markers. What is the most likely diagnosis?
-
What further management is advised?
Answers
1. Figure 2 shows extensive infiltration of lesional tissue with medium-sized cells with a high nuclear:cytoplasmic ratio, ‘salt-pepper’ chromatin and scant cytoplasm. There are numerous mitoses (black arrows) and apoptotic bodies (yellow arrows).
2. Histomorphological differentials would include lymphoma, neuroendocrine tumour or carcinoma. Immunohistochemistry would include: lymphoma markers – CD20, CD79a, CD3, CD10, BCL-6 & MUM1; neuroendocrine markers – CD56, synaptophysin and chromogranin; Ki67 growth fraction immunostain; and a pancytokeratin marker AE1/3 to exclude carcinoma.
3. Representative panels show the neoplastic cells staining positively for neuroendocrine markers CD56 and synaptophysin, characteristic ‘dot-like’ cytokeratin positivity and high Ki67 growth fraction. Lymphoma markers were all negative. The histomorphologic and immunhistochemical features are consistent with a METASTATIC NEUROENDOCRINE CARCINOMA to the orbit.
4. Full investigation including CT neck, thorax, abdomen and pelvis to locate the primary tumour, extent of disease and staging; neuro-oncology MDT discussion and referral to oncologist. Primary neuroendocrine tumours occur more commonly in the gastrointestinal or bronchopulmonary tracts. In this case, however, there were no lesions found at either of these sites. Furthermore, there were no liver metastases. The tumour may have originated in the ethmoid sinus and represent a primary sino-nasal neuroendocrine carcinoma which had locally invaded the orbit. CT scan revealed possible submandibular lymph node and T9 vertebral metastases. The patient is currently receiving chemotherapy.
The section editors would like to acknowledge and thank Mr Austin McCormick and Mrs Jean Hancock, Aintree University Hospital, for providing the clinical details.
COMMENTS ARE WELCOME




