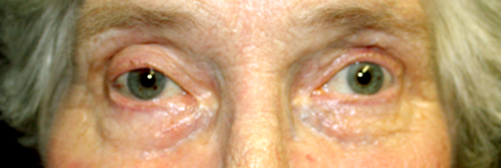
Figure 1: Photograph showing partial ptosis of the right eye two months after surgery (photo by R McLeod).
An 83-year-old lady had routine right eye cataract surgery under uncomplicated sub-Tenon’s anaesthesia. She presented two weeks later, explaining that following the removal of her eye pad on the same day of surgery she had been unable to open her right eye. When she manually opened her eyelid she was aware of binocular diplopia.
Examination demonstrated a right total ptosis, with right hypotropia and exotropia. The eye showed failure to adduct, elevate and depress. There was no anisocoria, and pupil reflexes were normal. Visual acuity was 6/9 and ocular examination on the slit-lamp was unremarkable.
A right (pupil-sparing) third nerve palsy was diagnosed. CT angiography was performed immediately and aneurysmal pathology excluded.
After two months there was only a partial ptosis and ocular movements were recovering (Figures 1 and 2).
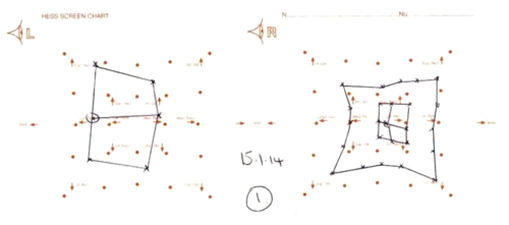
Figure 2: Hess chart demonstrating limitation of right eye movements after two months.
This lady therefore developed a third nerve palsy during the immediate perioperative period for cataract surgery, since the palsy manifested on removal of her eye pad. It is quite possible, given her age, that this is a microvascular event coinciding with cataract surgery. However, the striking temporal pattern does demand consideration that her sub-Tenon’s anaesthesia could be the cause of the third nerve palsy. Biological plausibility for this is difficult to theorise, but it has previously been reported that underneath the Tenon’s capsule is a lymph space, which follows the optic nerve and is continuous with the subarachnoid space, and that accidental injection of local anaesthetic agent into this part of the posterior sub-Tenon’s space can enter the subarachnoid space through the optic nerve sheath [1].
Diplopia has been reported as a complication of sub-Tenon’s block, when a presumptive diagnosis of inferior rectus fibrosis was made [2]. Traumatic muscle damage or local anaesthetic-induced myotoxicity were suggested causes. However, in our case, the experienced anaesthetic team reported the block as uncomplicated, with no evidence to suggest trauma or haematoma.
This is the first published report, to the authors’ knowledge, of a third nerve palsy occurring immediately after cataract surgery with sub-Tenon’s anaesthesia. This case demonstrates either a striking coincidence of microvascular neuropathy and cataract surgery, or possibly a rare complication of sub-Tenon’s anaesthesia.
References
1. Standring S, Ellis H, Healy J, Johnson D, Williams A. In Gray’s Anatomy: The Anatomical Basis of Clinical Practice 40th edn. Churchill Livingstone; 2008.
2. Blum RA, Lim LT, Weir CR. Diplopia following sub-Tenon’s anaesthesia: an unusual complication. International Ophthalmology 2012;32(2):191-3.
COMMENTS ARE WELCOME





