Melanocytoma is a heavily pigmented lesion, composed of melanocytes and is a variant of melanocytic naevus. It classically occurs at the optic disc and is usually benign, static and asymptomatic. However, it can occasionally grow and invade the retina or choroid and rarely it can transform into a malignant melanoma.
Case report
A 46-year-old man was referred to clinic via his optician for an opinion on “a raised, pigmented lesion” at the left optic disc. The patient was asymptomatic and had attended his optician for a routine sight check. He had no relevant past ocular or medical history and was not taking any medication.
On examination, visual acuity was 6/6 in the right and 6/6 in the left. Ocular movements were full, there was no diplopia in any position of gaze. Anterior segment examination was normal with the pupils reacting equally to light on both sides. On dilated ophthalmoscopy the right retina was normal. The left retina revealed an elevated pigmented lesion over the optic disc. The lesion was measured using B scan ultrasonography and found to be 2.4mm x 1.7mm. The clinical appearance of the lesion was consistent with a diagnosis of melanocytoma.
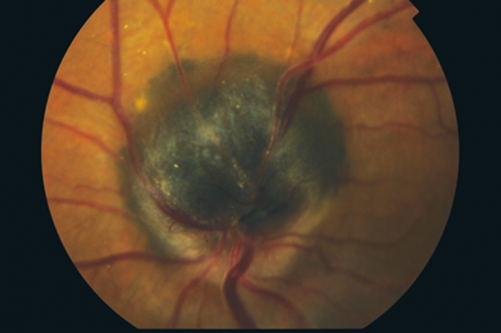
Figure 1: Optic disc melanocytoma.
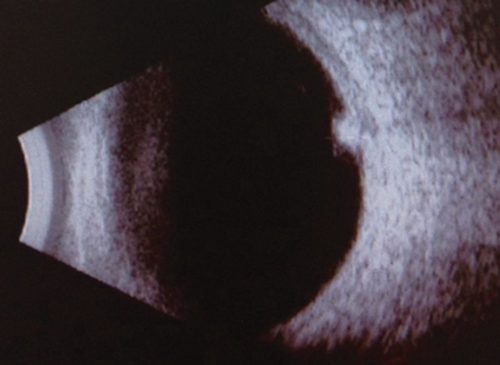
Figure 2: B scan of optic disc melanocytoma.
Comment
Melanocytoma was described and named by Zimmerman in 1962 [1]. It is defined as a specific variant of melanocytic naevus, located in the optic disc or anywhere in the uveal track characterised clinically by a dark brown or black colour [2]. Histopathologically, they consist of heavily pigmented cells with abundant cytoplasm and small, uniform bland nuclei [3]. Bilateral melanocytoma has been documented but is rare and occurs mostly in children [4].
The differential diagnosis of melanocytoma includes choroidal naevus, hyperplasia of the retinal pigment epithelium, metastatic melanoma to the optic disc and juxtapapillary choroidal melanoma [3]. Although very rare, primary malignant melanomas can occur at the optic disc and distinguishing from melanocytomas of the optic disc could be difficult or impossible clinically. Significant enlargement of the lesion and visual loss are suggestive of a malignant lesion but histopathology is often necessary for confirmation. Ocular melanocytoma has been associated with ocular melanocytosis [8]. No strong association with systemic diseases has been shown although some case reports suggest an association with intracranial meningiomas [9].
Diagnosis is based mainly on clinical appearance. B-scan helps to measure the lesion and monitor its growth. Fundus fluorescein angiography and indocyanine green angiography are of limited value due to the intense pigmentation of the lesion [3].
Melanocytomas do not usually result in visual loss, however, occasionally they can affect vision if the lesion extends to involve the fovea, causes focal subretinal fluid, intraretinal haemorrhage or retinal vascular occlusion [5]. The lesion can also undergo spontaneous necrosis, resulting in visual loss [7].
Melanocytomas may elicit paradoxical pupillary reactions, an afferent pupillary defect in the presence of very good visual acuity [3]. Patients may also present with field defects due to compression of the optic disc fibres by the lesion.
It has been reported that the initial thickness of the lesion has a predictive value for growth with lesions greater than 1.5mm at a higher risk of growth [8].
The patient in this case report was asymptomatic; this is typical of melanocytoma and most lesions are incidental findings [3]. In less than 2% of cases, melanocytomas may undergo malignant transformation [6], therefore, these lesions should be measured and documented at the initial visit and monitored annually to assess any growth.
References
1. Zimmerman LE, Garron LK. Melanocytoma of the optic disk. Int Ophthalmol Clin 1962;2:431-40.
2. De Potter P, Shields CL, Eagle RC, et al. Malignant melanoma of the optic nerve. Arch Ophthalmol 1996;114:608-12.
3. Shields JA, Demirci H, Mashayekhi A, et al. Melanoctyoma of the Optic Disk: A Review. Surv Ophthalmol 2006;51(2);93-104.
4. Gahankari MD, Jehangir R, Bhatti SS. Melanocytoma of the optic disc. J Postgrad Med 1992;38(3):135-6.
5. Takahashi T, Isayama Y, Okuzawa I, et al. Unusual case of melanocytoma in optic disk. Jpn J Ophthalmol 1984;28:171-5.
6. Zografos L, Uffer S, Gailloud C, Kohli M. Malignant melanoma of the optic disk, a case report. Klin Monatsbl Augenheilkd 1982;180(5):503-9.
7. Garcia-Arumi J, Salvador F, Corcostegui B, Mateo C. Neuroretinitis associated with melanocytoma of the optic disk. Retina 1994;14(2):173-6.
8. Shields JA, Demirci H, Mashayekhi A, Shields CL. Melanocytoma of optic disk in 115 cases: the 2004 Samuel Johnson Memorial Lecture, part 1. Ophthalmology 2004;111(9):1739-46.
9. Shinoda K, Hayasaka S, Nagaki Y, et al. Melanocytoma of the left optic nerve head and right retrobulbar optic neuropathy compressed by a tuberculum sellae meningioma. Ophthalmologica 2000;214(2):161-3.
COMMENTS ARE WELCOME





