A 74-year-old man had persistent 3+ cell one month following left eye cataract extraction, complicated by anterior capsular rent and zonular dialysis at 7 o’clock, with single-piece acrylic intraocular lens implantation (IOL) in the capsular bag.
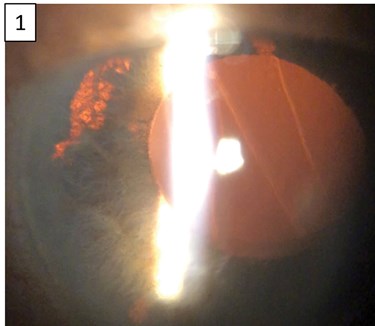
Figure 1: Haptic-like transillumination defect of the nasal iris.
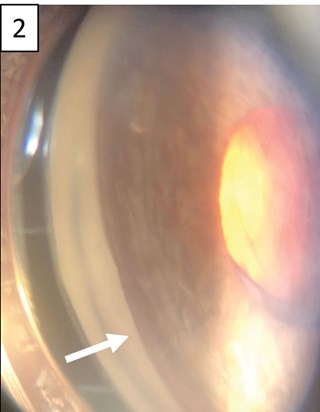
Figure 2: Dense pigmentation of the angle structures on gonioscopy.
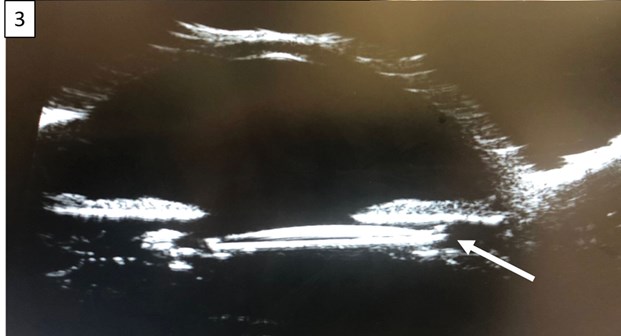
Figure 3: Ultrasound biomicroscopy demonstrated IOL decentration
and displacement of the superior haptic into the ciliary sulcus.
At one-month follow-up, the IOL was superiorly displaced with a haptic-like transillumination defect of the nasal iris (Figure 1). Gonioscopy of the left eye revealed dense pigmentation of the angle structures (Figure 2). Ultrasound biomicroscopy demonstrated IOL decentration and displacement of the superior haptic into the ciliary sulcus (Figure 3), resulting in persistent mechanical chafing of the posterior iris. Intraocular pressure was elevated to the mid-20s due to secondary pigment dispersion. The patient was taken to the operating room for lens explantation and secondary anterior chamber IOL placement.
Discussion
Single-piece acrylic IOLs that are displaced into the ciliary sulcus can cause issues. Some surgeons elect to perform ciliary sulcus implantation of a single-piece acrylic IOL following posterior capsular rupture when a three-piece IOL is unavailable, though multiple studies have encouraged surgeons to abandon this practice due to increased risk for uveitis-glaucoma-hyphema (UGH) syndrome [1,2]. This is because the bulky square-edged haptics of these IOLs can cause mechanical chafing of the posterior surface of the iris resulting in pigment dispersion and elevated intraocular pressure, iris transillumination defects and atrophy, microhyphema, and chronic inflammation. The potential for single-piece acrylic IOLs to cause UGH syndrome when they are displaced either partly or completely in the sulcus is well-recognised, yet the diagnosis is often missed early and medical management without lens exchange is rarely adequate [3-5].
References
1. Mohebbi M, Bashiri SA, Mohammadi SF, et al. Outcome of Single-piece Intraocular Lens Sulcus Implantation following Posterior Capsular Rupture during Phacoemulsification. J Ophthalmic Vis Res 2017;12(3):275-80.
2. Hong Y, Sun YX, Qi H, et al. Pigment dispersion glaucoma induced by the chafing effect of intraocular lens haptics in Asian eyes. Curr Eye Res 2013;38(3):358-62.
3. LeBoyer RM, Werner L, Snyder ME, et al. Acute haptic-induced ciliary sulcus irritation associated with single-piece AcrySof intraocular lenses. J Cataract Refract Surg 2005;31:1421-7.
4. Micheli T, Cheung LM, Sharma S, et al. Acute haptic-induced pigmentary glaucoma with an AcrySof intraocular lens. J Cataract Refract Surg 2002;28:1869-72.
5. Wintle R, Austin M. Pigment dispersion with elevated intraocular pressure after AcrySof intraocular lens implantation in the ciliary sulcus. J Cataract Refract Surg 2001;27:642-4.
COMMENTS ARE WELCOME





