A 67-year-old retired female nurse presented with persistent, bilateral, non-healing (>6 weeks) corneal ulcers and stromal ring infiltrates (Figures 1 and 2). The epithelial defects were the result of chemical burns caused by her contact lenses which had been stored in enzymatic cleaning solution.

Figure 1.
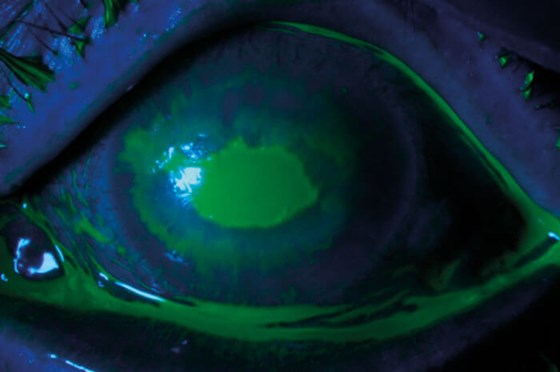
Figure 2.
Cornea samples were negative for herpes simplex, bacteria and fungi. A tarsorrhaphy was carried out in her left eye (Figure 3). Marked improvement was observed after one week (Figure 4). Prior to performing a tarsorrhaphy in her right eye, we noticed that the patient had been using anaesthetic drops for pain relief (Oxybuprocaine hydrochloride 0.4%). After cessation of the drops and a tarsorrhaphy, the right eye healed as well.

Figure 3.
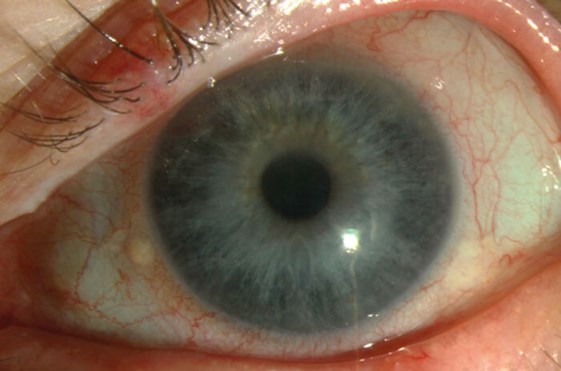
Figure 4.
Discussion
The cornea is one of the most densely innervated tissues in the body. Those dense corneal nerves and the neuropeptides produced by their fibres are essential for maintaining the health of the cornea [1]. Corneal nerves and epithelial cells mutually support each other by the release of trophic factors promoting epithelial cell proliferation, migration and differentiation, as well as nerve development and survival, all are necessary for a balanced ocular surface homeostasis and wound healing [2].
Neurotrophic keratitis is characterised by a reduction in corneal sensitivity, spontaneous epithelium breakdown and impairment of corneal healing.
Loss of corneal sensory function leads to a decrease in the vitality and metabolism of epithelial cells, and then to the breakdown of the epithelium and persistent defects [1]. In this case, tarsorrhaphy was beneficial for promoting epithelial regeneration and blocking the anaesthetic drops.
References
1. Cho KJ, Mok JW, Choi MY, et al. Changes in Corneal Sensation and Ocular Surface in Patients With Asymmetrical Keratoconus. Cornea 2013;32(2):205-10.
2. Versura P, Giannaccare G, Pellegrini M, et al. Neurotrophic keratitis: current challenges and future prospects. Eye Brain 2018;10:37-45.
COMMENTS ARE WELCOME





