Case report
Choroidal metastasis represents a common form of intraocular malignancies occurring in up to 10% of patients with systemic metastasis [1]. The most common primary sites of ocular metastasis are breast carcinoma in women and lung carcinoma in men, but may also include ovarian serous cystoadenocarcinoma [2] or multiple myeloma [3].
In most cases, these lesions tend to be asymptomatic and the diagnosis presents as an incidental finding. In some cases the choroideal metastasis may cause various visual disturbances, including complete loss of the vision secondary to a total retinal detachment. Combined pharmacotherapy with tamoxifen, cyclophosphamide hydrate, letrozole and bevacizumab is effective in the treatment of ocular metastases from breast cancer [4] and multiple intravitreal bevacizumab injections administered concurrently to systemic chemotherapy has demonstrated stability in a rare secondary ocular plasmacytoma case.
We present a case of a 52-year old Caucasian lady under the care of the oncologists with ER positive, HER-2 negative, invasive ductal carcinoma of the left breast. She had known metastatic dissemination of the breast carcinoma to liver, lung, bone and choroid bilaterally. The patient underwent a palliative cycle of gemcitabine and carboplatin chemotherapy (cycle six with good partial response) and was undergoing treatment with denosumab at the time of our ophthalmological assessment. She had bilateral choroidal metastases of her breast carcinoma in the past, which had been treated with bilateral orbital radiotherapy a year before. The radiotherapy treatment led to a good regression of the metastatic disease in both eyes but unfortunately the choroidal metastasis in her right eye had recently become active, leading to a total exudative retinal detachment (Figure 1).
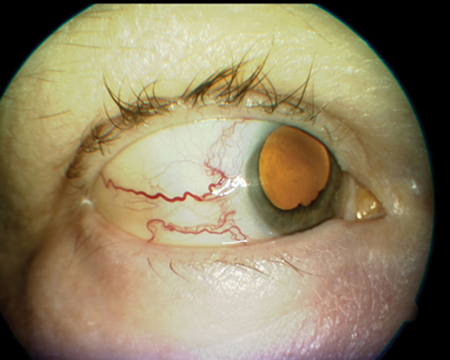
Figure 1.
The ophthalmological assessment demonstrated dilated sentinel vessels (Figure 2), which appeared to feed the choroidal metastasis, compatible with a resurgence in the activity.
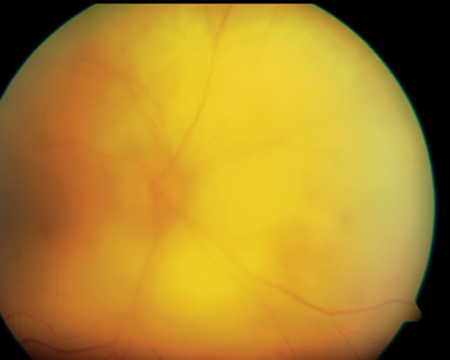
Figure 2.
Vision in the right eye was perception of light only due to a combination of total retinal detachment and dense cataract, and the intraocular pressure had increased to 26mmHg despite topical pressure lowering drops. The visual acuity of the left eye was 6/12. The patient was very keen to try to get back as much vision as possible in the right eye so, having already received the maximum tolerable dose of radiotherapy, locally delivered anti-VEGF therapy was planned with the aim to induce disease regression and some improvement in visual acuity in the eye. Exceptional funding was applied to administer a single intravitreal bevacizumab (Avastin) injection and after approval this was performed on the right eye.
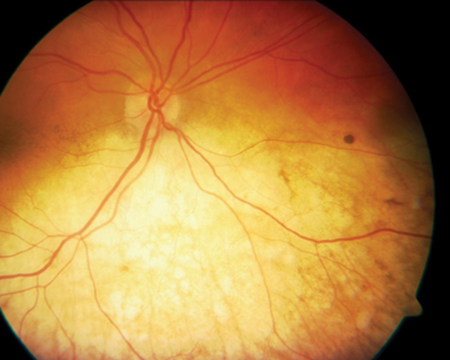
Figure 3.
Six weeks post treatment the patient reported subjective improvement of her vision up to counting finger and a subjective expansion of her visual field since her last visit. Examination revealed regression of the sentinel vessels, reduction in size of the metastatic lesion and complete resolution of the retinal detachment (Figure 3). The intraocular pressure also reduced to 9mmHg. A second bevacizumab injection was planned but unfortunately this was not possible because the patient died due to the primary disease.
Discussion
Management of ocular metastasis may vary from case to case. Small tumours not compromising the vision and responding to previous systemic treatment may be closely observed [1]. For larger and symptomatic lesions, external beam radiation is an excellent alternative treatment. Bevacizumab (Avastin) is a potent monoclonal antibody that has also been employed for the treatment of ocular vaso-proliferative diseases. When used intraocularly it has shown promising results in cases when utilised especially in high dosage (4mg/0.16ml) and in combined treatment with indocyanine green mediated photo thrombosis [5]. Our case report demonstrates that due to its availability and easy administration, even a single 1.25mg intravitreal bevacizumab proved to be a safe and effective ‘rescue’ treatment for choroidal metastasis from breast cancer that has not regressed after maximum tolerate radiotherapy, able to induce a regression of the secondary lesion as well as complete resolution of a co-existing exudative retinal detachment.
There are no clinical trials documented in literature so further studies should be conducted to confirm the appropriate dosing and long-term outcomes of intravitreal bevacizumab in the management of such lesions.
References
1. Giuliari GP, Sadaka A. Uveal metastatic disease: current and new treatment options (review). Oncol Rep 2012;27(3):603-7.
2. Kuo IC, Sambuelli RH, Bono J, et al. Progression of choroidal metastasis of ovarian serous cystoadenocarcinoma after intravitreal bevacizumab treatment. Rare Tumors 2013;5(1):e5.
3. Zhou Q, Liang J, Lu H. Intravitreal bevacizumab for ocular metastasis of multiple myeloma. Optom Vis Sci 2013;90(9):e236-40; discussion 1028.
4. Zako M, Takeyama M, Naito E, et al. Choroidal and optic disc metastases from breast cancer and their response to combination pharmacotherapy with tamoxifen, cyclophosphamide hydrate, letrozole, and bevacizumab. J Ocul Pharmacol Ther 2012;28(1):89-93.
5. Arevalo JF, Espinoza JV. Indocyanine green mediated photothrombosis and high dose intravitreal bevacizumab as adjuvant therapy for isolated choroidal metastasis from breast cancer. J Ophthalmic Vis Res 2012;7(4):332-40.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME





