Angioid streaks (AS) on their own do not cause many problems, with the majority of patients remaining asymptomatic [1]. However, once choroidal neovascularisation (CNV) occurs, the visual prognosis of the patient rapidly declines [2]. Treatment is imperative to try and improve visual acuity, as without it patients can be rendered legally blind [1,3-5]. Treatment has proved difficult, with some treatment modalities exacerbating the condition, and others only having a short-term effect [1,4,5]. We present a case successfully treated with a course of anti-VEGF injections.
Case report
Our patient was initially referred to check for AS at the age of 15, when she had been diagnosed with Pseudoxanthem Elasticum. She was found to have bilateral AS, and remained asymptomatic until the age of 39. She then presented with visual distortion and deterioration in her left eye. Visual acuity was 6/5 bilaterally, anterior segment was normal as were both intraocular pressures (IOPs). She was found to have left macular elevation, left subretinal elevation and subretinal haemorrhages (Figure 1). An urgent fundus fluorescein angiography (FFA) showed CNV in the left eye. She was commenced on a course of three anti-VEGF injections in her left eye, with intervals of four weeks.
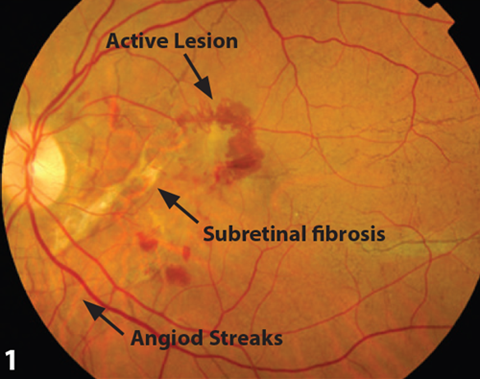
Figure 1: Fundal photo demonstrating active lesion and angiod streaks.
After treatment her vision improved by four lines on logmar, the sub-retinal fluid was resolving bilaterally, and there was evidence of sub-retinal fibrosis in the left eye. Changes in optical coherence tomography (OCT) and FFA are demonstrated in Figures 2-5.
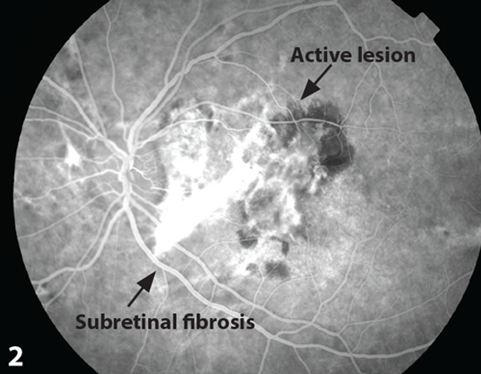
Figure 2: Active lesion demonstrated during aterio-venous phase of FFA, pre-treatment.
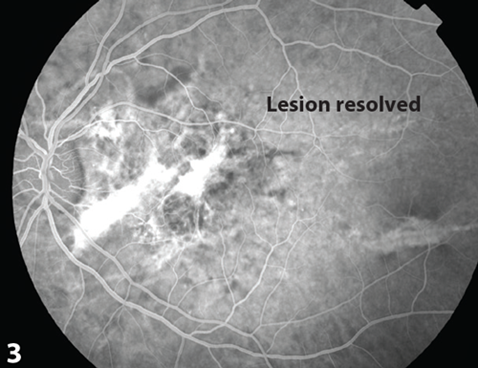
Figure 3: Resolution of lesion demonstration durring aterio-venous phase of FFA, post-treatment.
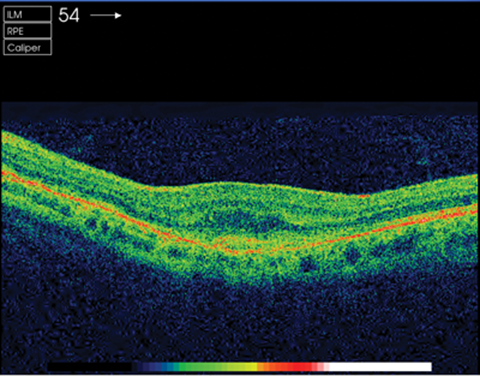
Figure 4: OCT pre-injection.
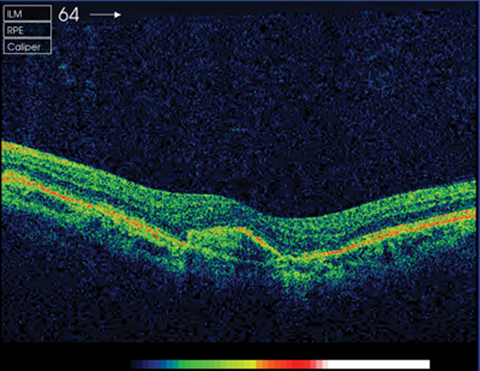
Figure 5: OCT post-injection. © Hanif Patel, Retinal Photographer.
She remained stable for one year, after which she felt the vision in her right eye was deteriorating. Visual acuity remained at 6/6 in her left, and had marginally decreased in her right to 6/7.5. OCT revealed early thickening of the pre-retinal membrane in the right eye. She was later found to have early macular leakage on FFA and evidence of CNV. She has been commenced on another three injection course of anti-VEGF in her right eye, and it is hoped that vision in her right improves and remains stable, like that of her left.
Comment
Angioid streaks were first described in 1889 by Doyne, and named by Knapp in 1892, who suspected they were the result of vascular pathology [1,2]. It was later revealed they occur as a result of breaks in Bruch’s membrane, which is abnormally brittle in these patients [1]. AS is associated with numerous conditions, and is thought to have a familial component (our patient has a sister with AS, but no systemic association) [2,6].
The majority of patients remain asymptomatic until they develop a complication, the most common of which is CNV [1,3-5]. Between 72% and 86% of patients will develop CNV in one eye, with 71% going on to develop CNV in the other eye, after roughly 18 months [1,3,4]. CNV is thought to occur as blood vessels are able to extend through the breaks in the membrane [5] and without treatment the patients can become severely visually impaired [1,4]. However, treatment of CNV in angioid streaks has proved difficult (Table 1). Although numerous treatment modalities have been trialled, they have had limited success. Photodynamic therapy and photocoagulation have been shown to have short-term effects and high probability of recurrence. Macular surgery appears promising, but is a lengthy process with numerous complications [1].
The most promising treatment in these scenarios seems to be anti-VEGF. There are several papers looking at anti-VEGF in these patients, and it appears to be relatively safe, and is the most likely to both improve, and stabilise vision [1,3-5].
All patients with AS should be closely monitored. Patients complaining of distorted or decreased vision should be investigated, as this implies macular involvement. Treatment should be initiated to try and preserve vision, but even those treated with anti-VEGF, may have a guarded visual prognosis.
References
1. Georgalas I, et al. Angioid streaks, clinical course, complications, and current therapeutic management. Ther and Clin Risk Manag 2009;5:81-9.
2. Keith CG. Angioid streaks and pseudoxanthoma elasticum. Brit J Ophthal 1956;40:480-6.
3. Teixeria A, et al. Choroidal neovascularisation treated with intravitreal injection of bevacizumab (Avastin) in angioid streaks. Acta Ophth Scan 2006; 84(6):835-6.
4. Wiegand TW, et al. Intravitreal bevacizumab (Avastin) treatment of choroidal neovascularisation in patients with angioid streaks. Brit J Ophthal 2009;93:47-51.
5. Rinaldi M, et al. Intravitreal bevacixumab for choroidal nerovascularization secondary to angioid streaks. Arch Ophthal 2007;125(10):1422-3.
6. Hull D, et al. Fluorescein study of a family with angiod streaks and Pseudoxanthem Elasticum. Brit J Ophthal 1974;58:738-45.
7. Pece A, et al. Laser photocoagulation of choroidal neovascularization in angioid streaks. Retina 1997;17:12-6.
8. Singerman LJ, et al. Laser treatment of choroidal neovascular membranes in angioid streaks. Retina 1981;1:75-83.
9. Clarkson JG, et al. Angioid streaks. Surv Ophthalmol 1982;26:235-46.
10. Browning AC, et al. Verteporfi n photodynamic therapy of choroidal neovascularization in angioid streaks: one-year results of a prospective case series. Ophthalmology 2005;112:1227-31.
11. Shaikh S, et al. Photodynamic therapy using verteporfin for choroidal neovascularization in angioid streaks. Am J Ophthalmol 2003;135:1-6.
12. Ladas ID, et al. Photodynamic therapy with verteporfin of choroidal neovascularization in angioid streaks: conventional versus early retreatment. Eur J Ophthalmol 2005;15:69-73.
13. Aras C, et al. Two cases of choroidal neovascularisation treated with transpupillary thermotherapy in angioid streaks. Retina 2004;24:801-3.
14.Tanaka M, et al. Surgical removal of choroidal neovascularization in angioid streaks. Nippon Ganka Gakkai Zasshi 2003;107:440-4.
15. de Juan E Jr, et al. Limited macular translocation. Eye 2001;15:413-23.
16. Roth DB, et al. Macular translocation for subfoveal choroidal neovascularization in angioid streaks.
Am J Ophthalmol 2001;131:390-2.
17. Wecke T, et al. Intraocular injections of bevacizumab in rare indications – two cases. Ophthalmologe 2009;106(5):435-42.
18. Chang LK, et al. Bevacizumab treatment for subfoveal choroidal neovascularization from causes other than age-related macular degeneration. Arch Ophthalmol 2008;126:941-5.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME





