This edition’s survey questions moved away from the deep and ethically charged questions of the recent surveys and focussed on simple and straightforward issues. This is really where the surveys began in exploring the minor practice variations which we have all fallen into and questioning why we have the variance and whether this will have an impact on patient care.
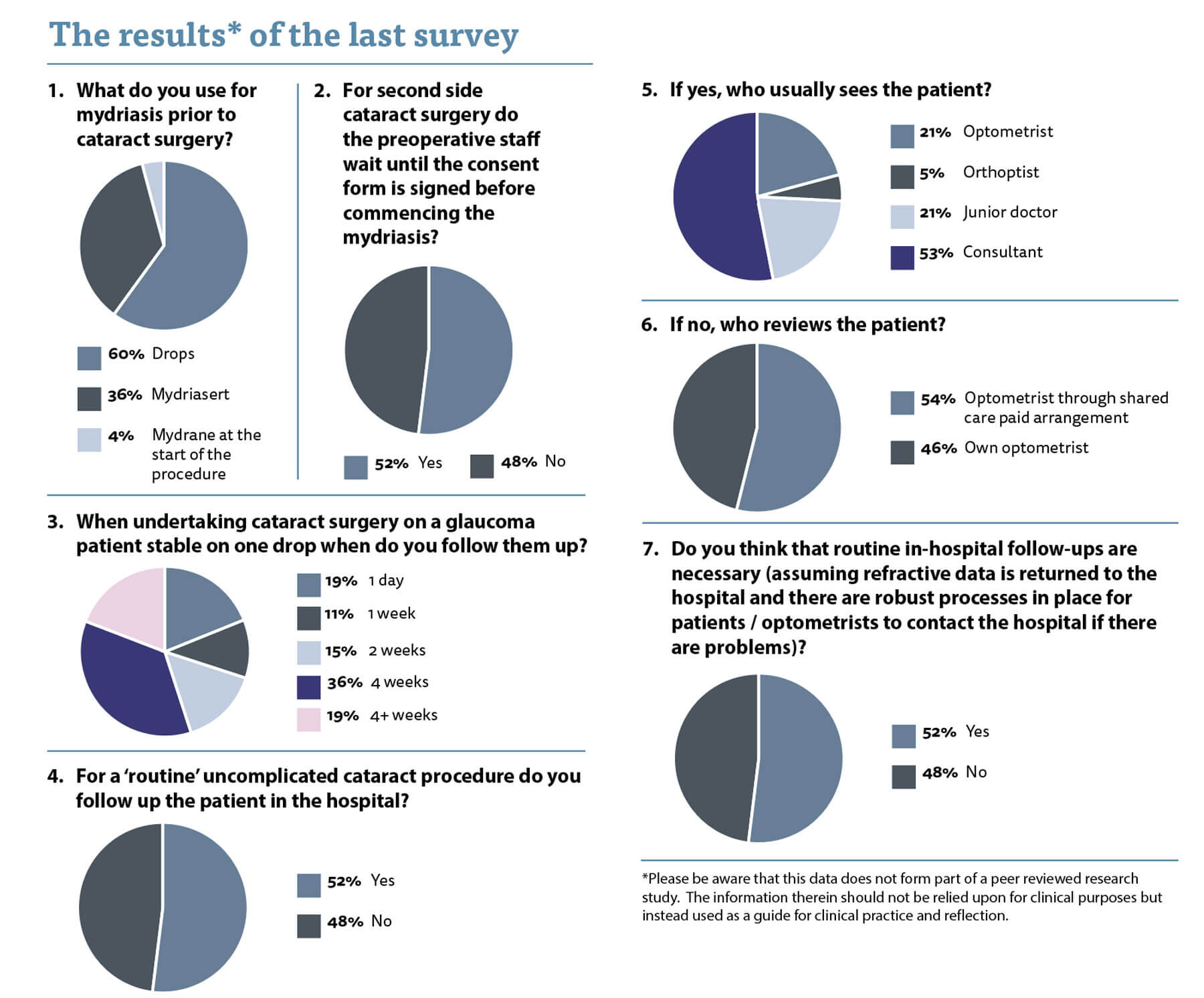
The first question relates to mydriasis for cataract surgery and how this is achieved. Sixty percent of us use drops, whereas 36% use a mydriatic pellet. I used to use dilating drops but the workload for the nursing / admitting staff was very high and I have found it much more efficient to use the Mydriasert™ pellets to achieve good pupil dilatation. A small minority of us use the Mydrane™ and despite some rave reviews from some surgeons I have been disappointed by the efficacy of it as a stand-alone method for achieving preoperative mydriasis.
The second question relates to an issue I face on occasion on my lists. Some of the nursing / admitting staff insist on waiting until the consent form is signed before they will administer the pellets for mydriasis. I have a high-volume cataract list and sometimes we can have most of the list filled with second eyes. Delaying the pellet administration until I have seen the patient causes significant delays to my operating list. Indeed, I have had occasions where the pupil was still reactive on the table as the mydriatic pellet had only been placed in the eye five minutes before they were brought to theatre.
I am happy for my patients to have their mydriasis prior to my seeing them. They are second eye patients and so they know which eye they had done first. The patient’s opinion about which eye they are having done should match the operating list and if it does not then this should be flagged up to me to investigate before they have their dilatation protocol commenced. If there is agreement between the operating list and the eye the patient indicates is being done, then I have no problem with commencement of mydriasis. I still check myself in the clinical record and confirm that the planned eye is correct eye and check with the patient. I also mark the patient. I have never had a situation whereby the patient points to the eye that has already been done and the operating list was also incorrect, but it could happen and we need to remain vigilant to that and ensure we are robust in our checks. If I discover that the wrong eye has been dilated, we can simply remove the pellet and the patient will not have come to any significant harm. This compares with the real risk of harm of operating on a patient with a pupil with incomplete mydriasis.
There was an almost 50:50 split in opinion and it is hard to know who is right. In actuality, there was a 52% to 48% split in opinion on this topic and if we stick by Brexit rules it means that we must all wait until the consent form is signed before we dilate the patient! (Clearly my Brexit bitterness is still strong.)
When asked when clinicians follow patients up after routine cataract surgery on a glaucoma patient there was surprising variance. A fifth of you followed the patient up on day one. Ten percent saw the patient at one week postoperatively, while 15% saw the patient at two weeks. More than a third checked the patient at a month and almost 20% even allowed longer. My practice is two weeks as I feel uncomfortable leaving the intraocular pressure (IOP) unchecked for longer and although it is early for a steroid response I still worry about it. I myself published the largest data series of day one follow-ups on routine glaucoma and non-glaucoma phacoemulsification cases and found that an IOP of more than 30mmHg was found in 5.1% of cases and was strongly associated with a diagnosis of pre-existing glaucoma or ocular hypertension (odds ratio [OR] 7.7) [1]. Symptoms of headache or ocular discomfort occurred in 40 (7.8%), mostly in association with raised IOP, and were also associated with pre-existing glaucoma or ocular hypertension (OR 4.7). My conclusion was that first day review may be omitted but in those patients with glaucoma this should be done with caution.
To bring us back to the underlying motive for this series, which is to determine, or at least give food for thought, as to whether varying from an ‘accepted’ practice can be deemed to be a breach of duty or not. For example, almost 20% of surgeons who responded said that they would leave glaucoma patients for more than a month postoperatively until they had an IOP check. If a glaucoma patient was found by their optometrist to have an IOP at week four of 45mmHg with worsened glaucoma, is that a breach of duty in not arranging more appropriate / earlier follow-up?
Again, we had a Brexit split on the issue of follow-up for routine patients after their cataract surgery. I personally do not think that patients need to be seen in the hospital after their surgery. I believe the safety profile is so good and the pick-up rate of problems at a routine follow-up so low. They go back to their optometrist anyway for refraction and new spectacles, so it makes sense they use their skills to assess the eye for us. Avoiding extra visits to the hospital is also more important now in the era of COVID-19. We also need feedback on refractive outcomes, vision and the presence of any postoperative issues and some optometrists would like renumeration for this extra work. I prefer to leave those discussions to the managers and commissioners. I note more than 50% of those who did send the patient to their optician for follow-up had some form of paid shared care arrangement.
If the patient did come back to the hospital for review, then in more than 50% of cases they were seen by the consultant. I am all for continuity of care but wonder whether consultants should be seeing routine postoperative patients or should be focussing their skills on the complex patients.
Once again, food for thought and reflection on practice.
Reference
1. Alwitry A, Rotchford A, Gardner I. First day review after uncomplicated phacoemulsification: is it necessary? Eur J Ophthalmol 2006;16(4):554-9.
Do you have a question you would like asked? Please email AmarAlwitry@btinternet.com
COMMENTS ARE WELCOME






