Thank you so much again for participating in the survey. I have been asked to give several talks at regional teaching sessions about some of the issues I discuss in these articles and I am happy to continue to do so. It is vital that we continue to challenge, evolve and improve our practice.
A wrong intraocular lens implantation is a never event and should not occur. When it does happen, it is usually due to a sequence of errors resulting in the perfect storm of errors.
Often I have asked you questions where there is no real guidance available but in this case there is guidance. The Quality Standard from the Royal College of Ophthalmologists ‘Correct IOL implantation in cataract surgery’ was published in March 2018.
I write the IOL power on the board and where I will place my corneal incision as I prefer on-steep-axis surgery. I write down all my IOL powers on my operating list as I am seeing and marking my patients. I then transcribe that to the whiteboard as a triple check mechanism. When we check the IOL we check the notes and the biometry, then look at the whiteboard, and aloud state “20 dioptre circled on biometry, 20 dioptre written on the board and 20 dioptre lens got.” I appreciate the argument is that we leave ourselves open to transcription errors, however, the number on the board is not the only check and it has to tally with the biometry. If there is a discrepancy it gives us a chance to stop and reassess where it has come from.
The guidance states: “Consider circling or highlighting the correct IOL model and power required on the source biometry print out page. This needs to be signed or initialled / dated and traceable.”
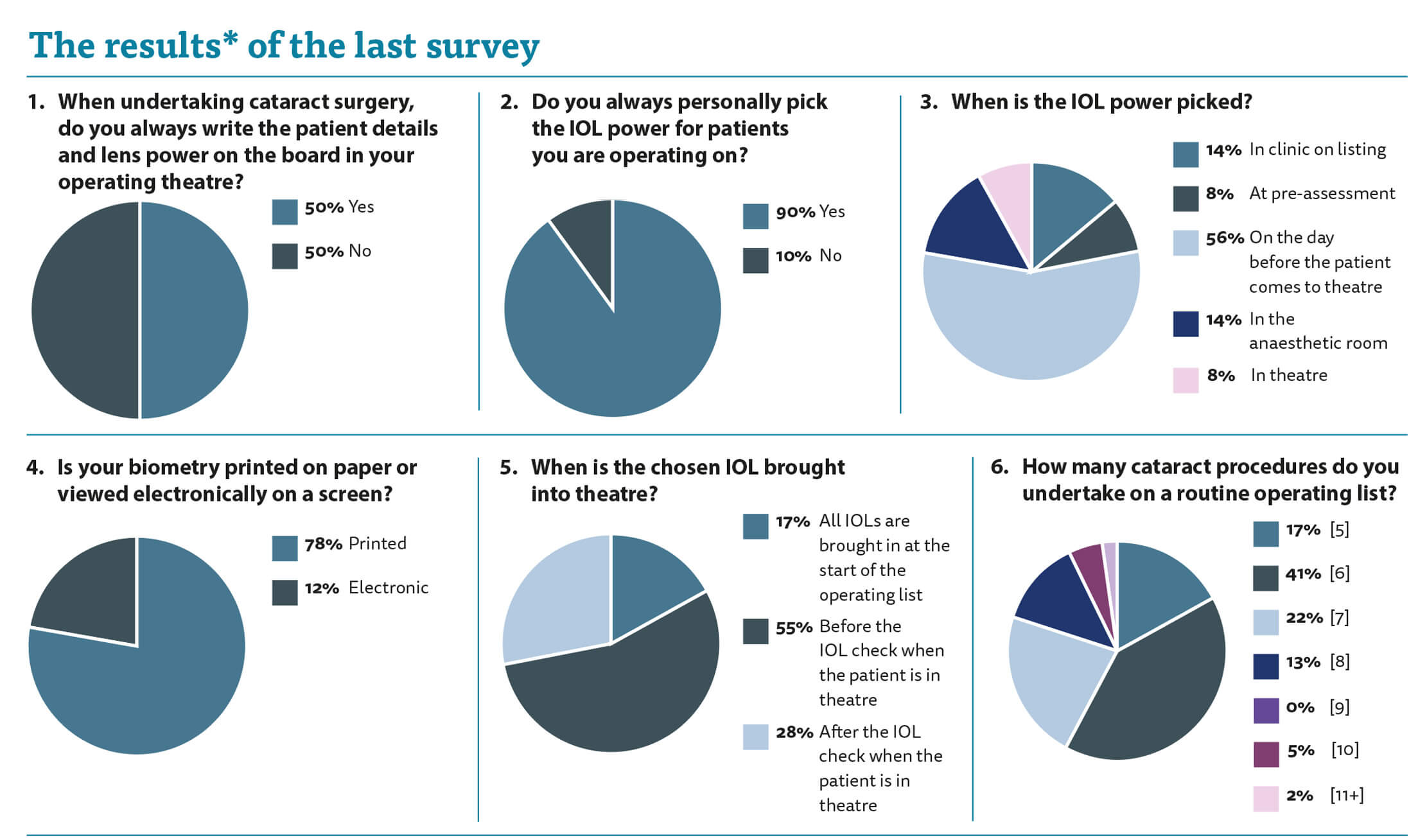
Interestingly, it also states: “Minimise use of operating theatre ‘white boards’ and, if using theatre lists or white board transcription for recording IOL selection, all checks must also consult the source biometry printout.” It is guidance and I have a rationale for using my methodology so I will stick with writing my surgical plan on the whiteboard. Half of you agree with me and half of you do not use the whiteboard.
When asked who picks the IOL power I was surprised to see that in 10% of cases someone else picks it. I appreciate that you recheck it yourselves, but you leave yourselves wide open to confirmation bias whereby you will simply rubber stamp the original IOL choice. And who takes the blame if the wrong IOL is chosen, the operating surgeon, or person who picked the IOL?
The guidance says: “IOL selection should be performed by the operating surgeon if possible, or by a suitably trained clinical professional to be confirmed by the operating surgeon.” Personally, I think we should be picking the IOL power ourselves.
When asked about the timing of the IOL choice there was a spread of opinion. In 14% the lens was chosen in clinic on listing. I can appreciate this. You have just spoken to the patient and discussed their refractive outcome so everything is fresh in your mind. My worry, as mentioned above, is that you may not be operating upon the patient yourself and so you are picking an IOL for another surgeon who should really be refining their IOL power choice with their personalised A-constant.
The guidance clearly states: “IOL selection should take place during the assessment clinic or in the preoperative ward-round.” And: “IOL selection performed during the assessment clinic should be checked at the preop ward round on the day of surgery.”
Sixty-four percent of respondents chose the IOL power at the pre-assessment visit or on the day before the patient comes to theatre and, personally, I feel this is best practice. Twenty-four percent of you chose the IOL power in the anaesthetic room or in theatre. I worry that this is leaving the door open for error. You are in the midst of doing several things and you are not focussed on the notes, the measurements and the biometry.
Seventy-eight percent of you are old fashioned and have the biometry on paper rather than on a screen. I like having the paper biometry there so I can physically look at it when we are checking the consent form and confirming the patient details.
When asked when the IOLs are brought into theatre I was surprised to see that 17% of you have all the IOLs brought into theatre at the start of the list. I seem to spend my nights sleepless and worrying about you all and this adds to the list of concerns. Again, we are prone to confirmation bias. If the IOL is in the room then we are more likely to assume it is the correct one. If the list order changes then can we be confident that the IOL will change its position in the queue too?
I think it is much safer to have only one IOL (the IOL for that patient) in the operating theatre at a time. The guidance states: “Check lens and backup are available and only one lens is in theatre prior to anaesthetic. There should only be one lens out in theatre at any one time.”
I wonder why we have one off guidance and then no reminders? How many of you have read the guidance I refer to above? Is there a mechanism whereby we can be reminded of these recommendations? We will sadly be criticised for not following the guidance and yet how often are we nudged to look at it again?
My last question shows the variance of numbers of cataracts done on each operating list. Fifty-eight percent of you do five or six cataracts on a list. Thirty-five percent did seven or eight, while only 7% did more than that. We each work at different speeds but it does make me wonder about the processes that surround our operating and whether these could be improved to standardise productivity and improve throughput for the benefit of the health economy as a whole.
*Please be aware that this data does not form part of a peer reviewed research study. The information therein should not be relied upon for clinical purposes but instead used as a guide for clinical practice and reflection.
Do you have a question you would like asked? Please email AmarAlwitry@btinternet.com
COMMENTS ARE WELCOME






