Once again, I am grateful for the responses and read the results with interest.
I am always surprised by the amount of practice variation I see. I fully accept there is art in what we do and there is no one size fits all regarding our practice. We each have different experience and we do the things that work best for us and our patients. We are not robots but surgeons, so we will inevitably do things differently.
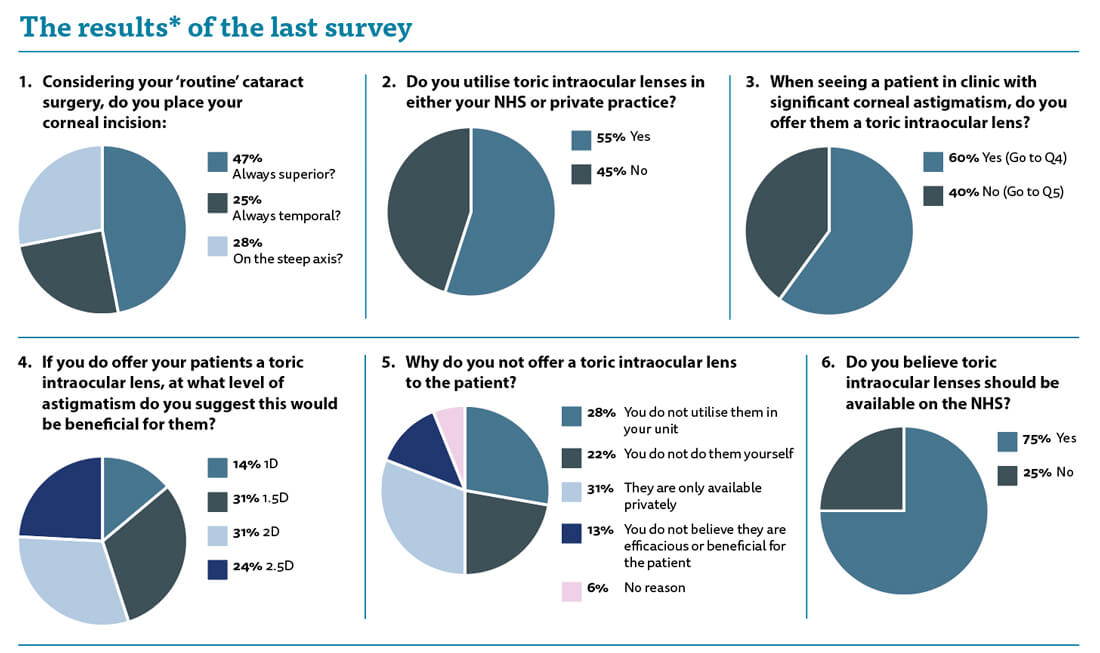
When asked where you place your corneal incision, we seemed to have an even spread across all the responses. Patients are getting more demanding with time and are keener than ever to achieve a good refractive outcome. My practice is that I always try and put my incision on the steep axis of the cornea to try and reduce pre-existing astigmatism and that sounds ideal, but in practice it is not always so simple. Not everyone has a set up that facilitates temporal incisions if they are needed. In one of the hospitals where I work there is not enough room in the theatres to sit at the side, so I am forced to sit at the top to operate. If possible, we should consider the patient’s astigmatism and try to reduce it if we can. I have seen many patients in my clinical and medicolegal practice who are unhappy with an increased amount of astigmatism and often this induced astigmatism forces them to wear spectacles when they did not need to for distance before.
In the interests of openness, I have to say that I am a toric intraocular lens (IOL) fan and use them extensively in my private practice. I believe that the quality of vision the patients will achieve is better than correction with spectacles or contact lenses. We are obliged to offer patients any treatments which we think would be beneficial to them.
First, and foremost we must believe that the potential IOL we seek to discuss is indeed in the patient’s best interests. There is evidence to support the use of toric IOLs to reduce postoperative astigmatism [1,2], however, this only really refers to the benefit in being less spectacle dependant for distance. This may or may not be desirable for the patient, but it should be easily elucidated from questioning.
Guidance from the British Medical Association is clear [3]: “If treatment is only available privately, patients should be told that. Patients are generally aware of the availability of private treatment and so the option is always open to them to enquire, but where there is a new treatment available that is not provided on the NHS, patients cannot be expected to know about it. Therefore, it is appropriate to provide balanced and factual information about the treatment, although this needs careful handling to ensure the patient or the family do not feel pressure to choose the private option.”
If a clinician believes that the patient would benefit from an alternative treatment not available on the NHS it is reasonable to inform the patient of this option and encourage them to explore it further if they wish through private means. In practice this means asking the patient as part of a partnership approach, however, without making judgments the clinician should still use their clinical acumen. If a patient has a cylinder of 1D then it may be possible to address this quite easily with appropriate incision position or a limbal relaxing incision. If a similar patient has 3D of corneal astigmatism, then the likelihood is that they will be left with visually significant residual astigmatism and therefore a brief discussion regarding the benefits of toric IOLs is ethically appropriate.
It is inappropriate to deny patients choice and surgeons should not make decisions based on perceived willingness or affordability to decide whether to mention other treatment options.
In our survey, 55% of us do use toric lenses so they are widely available. When faced with a patient with significant corneal astigmatism, 40% of us do not offer them the toric option.
When asked why, 28% of respondents said it was because they were not utilised in their unit, 22% stated that it was because they did not use them personally, and 31% did not offer them to the patient because they are only available privately. We have to be careful not to act as salespeople and patients can be easily misled with the offers of “better” vision, when actually it is better vision without spectacles we are offering them. The use of spectacles postoperatively is not an issue for the vast majority of patients, but this is not a judgment we should assume by default.
When asked what sort of astigmatism would prompt discussion of a toric lens, 14% responded 1D or more, 31% felt that 1.5D was the threshold, whereas 31% and 24% felt that astigmatism above 2D and 2.5D respectively were needed before consideration of toric IOLs.
My experience is that if we can maintain a post-op astigmatism of less than 1D the patients tend to be happy. By placing my incision on the steep axis and titrating the height of that incision up the cornea depending on the degree of astigmatism I can get most patients with a cylinder of 1.5D or less below 1D postoperatively. I tend to discuss toric IOLs for patients who have a corneal cylinder of more than 1.5D.
As ever, the purpose of my editorials are not to give definitive guidance but food for thought and practice reflection.
References
1. Lake JC, Victor G, Clare G, et al. Toric intraocular lens versus limbal relaxing incisions for corneal astigmatism after phacoemulsification. Cochrane Database of Systematic Reviews 2019;12:CD012801.
2. Kessel L, Andresen J, Tendal B, et al. Toric Intraocular Lenses in the Correction of Astigmatism During Cataract Surgery. A Systematic Review and Meta-analysis. Ophthalmology 2016;123:275-86.
3. The interface between NHS and private treatment: a practical guide for doctors in England, Wales and Northern Ireland. Guidance from the BMA Medical Ethics Department, May 2009.
*Please be aware that this data does not form part of a peer reviewed research study. The information therein should not be relied upon for clinical purposes but instead used a guide for clinical practice and reflection.
COMMENTS ARE WELCOME






