We are often referred patients noted to have an optic disc haemorrhage (ODH) without any other features of pathology. How we manage these patients can have a significant impact on our struggling capacity.
The significance in glaucoma and, in particular, normal tension glaucoma (NTG) is well-known and it seems clear that the presence of an ODH can be a marker for progression and warrants a tighter follow-up, however, the situation in a de novo patient who does not have glaucoma is less clear.
The Bridlington Eye Study [1] found a prevalence of ODHs in eyes without glaucoma of 0.93%, so almost 1 in 100 normal patients will have an ODH. Should all such patients be referred into the hospital eye service and, if clinical examination was normal, should the patient be followed-up?
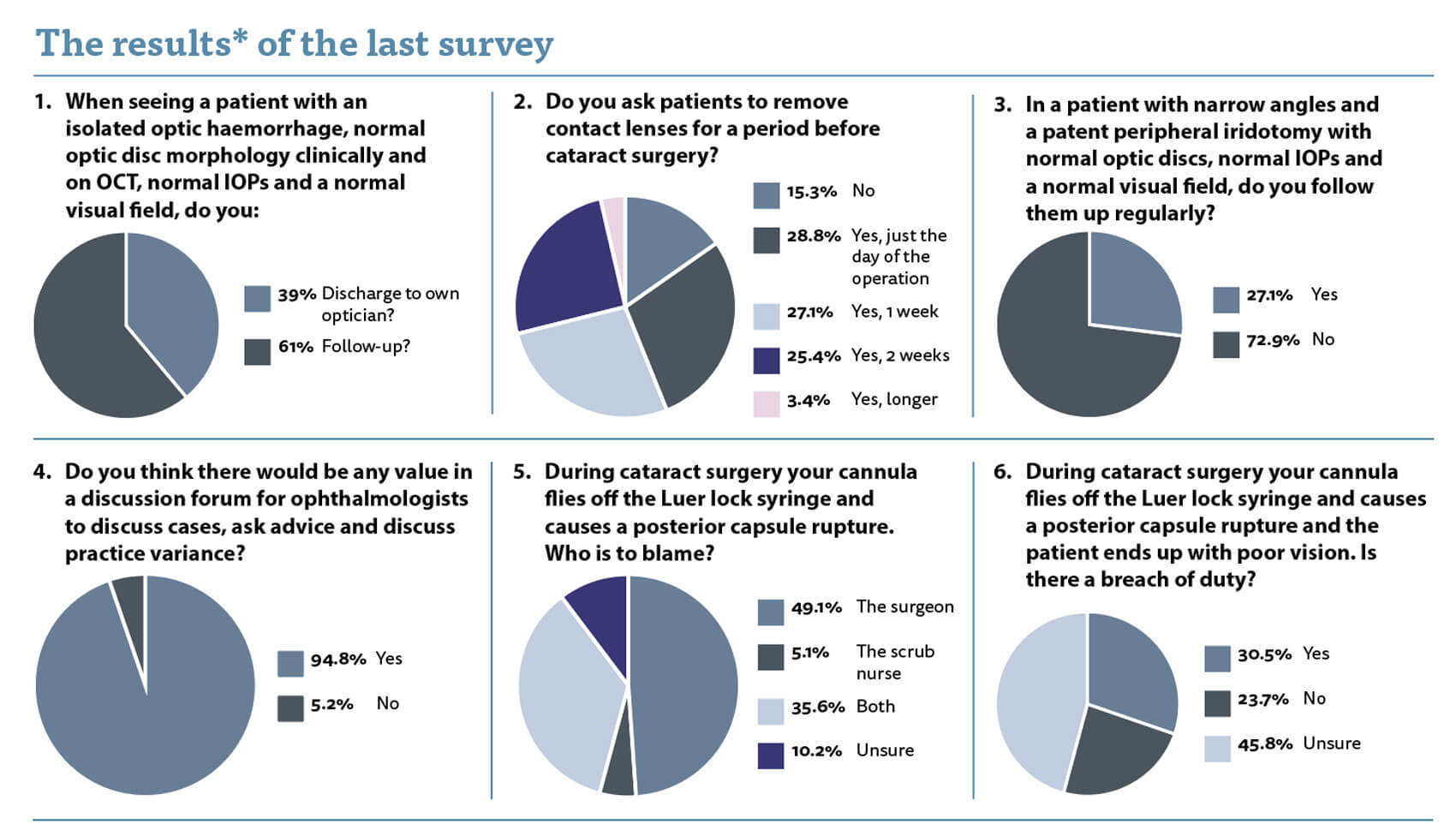
We are split in our management of this, with 39% of us discharging the patiet to their own optician, whereas 61% of respondents would follow the patient up. My personal practice is that I follow the patient up once at six months after the initial assessment with a visual field test and an optic disc OCT scan. My rationale is that I need to exclude the start of NTG. I know that an ODH can be a marker for progression of glaucoma and that there can be a lag between the visualisation of the ODH and the NFL loss. Unless I give my naïve patient a chance to progress, I cannot be sure that they are not starting to develop NTG. I thus see them once more to exclude NTG. I have not audited my pick-up rate for NTG and thus it is hard to analyse my practice. I wonder whether I need to see them myself or whether their optometrist could do just a good as job of following them up?
I often get asked whether a patient coming for cataract surgery should remove their contact lenses before surgery. I know the answer for biometry, but what about the surgery itself? Again, we are split. There seems to be an equal distribution of opinion between day before, one week and two weeks or longer. What is the evidence base for these decisions? I guess that those who want the lenses out for longer worry about corneal ischaemia or the risk of infection, but it has never been an issue for me and I am happy with patients keeping their contact lenses in until the day before surgery. I am happy to be educated.
When asked about follow-up for a patient with narrow angles and a patent peripheral iridotomy (PI) with normal optic discs, normal IOPs and a normal visual field, the majority of clinicians (73%) will discharge the patient to their own optician for follow-up. I think this is reasonable as any follow-up is surely to detect raised pressure despite the patent PI, which the patient’s optometrist is very capable of detecting at the annual sight test.

Figure 1: The ‘finger of safety’.
I still see regular incident reports and litigation cases surrounding the cannula flying off in the eye causing intraocular trauma. The hyrdraulic pressure / force generated is quite significant and the cannula can fly off with considerable momentum. It can be a blinding injury and is entirely avoidable. I recommend everyone has a ‘finger of safety’ (Figure 1) on the cannula when they are using it. This means that if the cannula does come loose, it simply rotates and falls off rather than being ejected with force.
So who takes the blame for the loose cannula if it does fly off? Half of respondents said the operating surgeon, a third said both, which I think is reasonable and only 5% felt the scrub nurse was to blame. Ten percent were unsure and I do not blame them. We all have a duty of care to the patient to prevent harm. As ever, with clinical errors, it is a sequence of events which lead to mishap. The scrub nurse failed to tighten the cannula and the surgeon failed to check and retighten. Furthermore, the surgeon failed to undertake precautions to ensure that if the cannula did come away it would not enter the anterior segment at speed. So we all materially contributed to the harm which would meet the legal standard for a breach of duty.
When questioned about whether you felt duty was breached, 30% said yes, 24% said no and almost 46% were unsure. Again, I do not blame those on the fence but if ophthalmologists are unsure then how will the court react? Let’s not get into that situation and ensure that we check the syringe and cannula for tightness and put a finger of safety on the cannula to minimise injury if a loose one slips through the net.
My fourth question refers to my long-standing desire to have some sort of forum whereby clinicians can ask questions of each other. I know there is a clinical leads forum run by the RCOphth, however, I think it would be great if there were a similar forum for ordinary ophthalmologists. We are all computer savvy and communications and social media are easy to access, and yet we learn and discuss in silos. I personally would value a forum where ordinary ophthalmologists can ask questions of each other without fear of ridicule or criticism. Why do you follow-up your patients with narrow angles and PIs? Do you cancel patients with uncontrolled blood pressure? I’ve got a patient with intractable cystoid macular oedema post cataract surgery, what would you do at this stage? Or even, my managers are asking me to only check intraocular pressures with an iCare tonometer and not Goldmann applanation tonometry, what do you think? We are a reasonably small speciality and I think we should learn, work, advance the science of ophthalmology and, most importantly, keep patients safe, together. Ninety-five percent of you seem to agree.
Reference
1. Wilde C, Poostchi A, Narendran R, et al. Prevalence of optic disc haemorrhages in an elderly UK Caucasian population and possible association with reticular pseudodrusen—the Bridlington Eye Assessment Project (BEAP): a cross-sectional study (2002–2006). Eye 2019;33:580-6.
*Please be aware that this data does not form part of a peer reviewed research study. The information therein should not be relied upon for clinical purposes but instead used as a guide for clinical practice and reflection.
Do you have a question you would like asked? Please email AmarAlwitry@btinternet.com
COMMENTS ARE WELCOME






