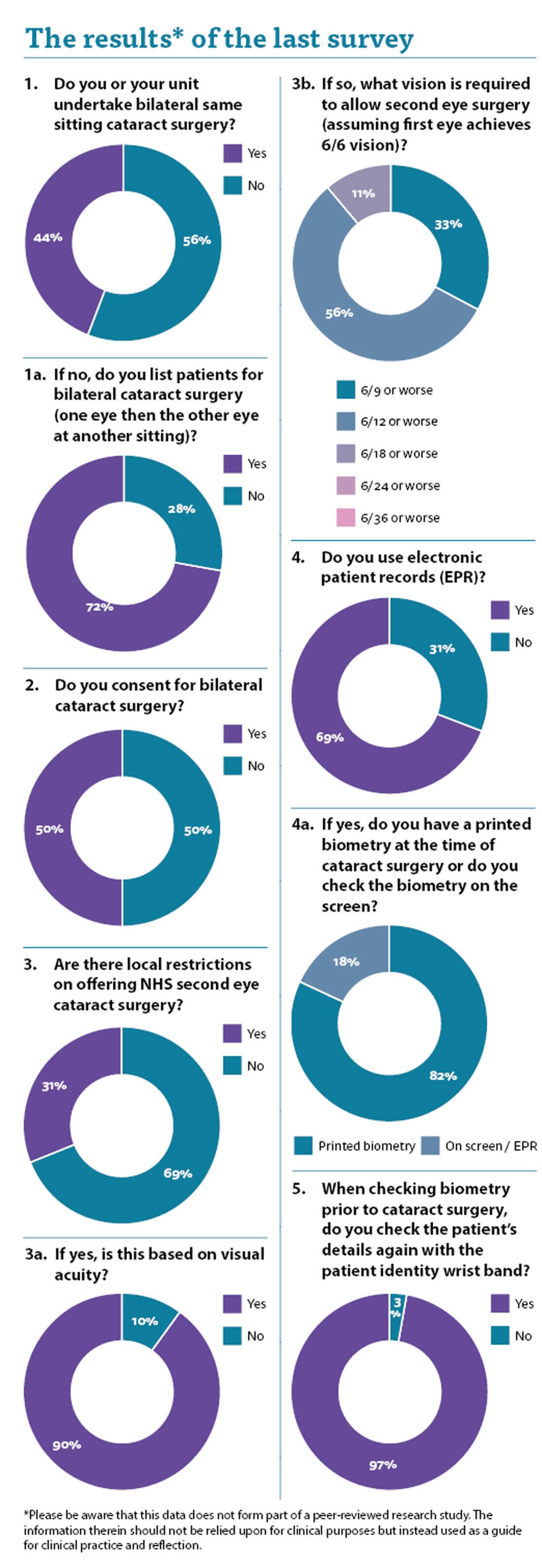
The answer to the first question was interesting in that it seems an increasing number of units are doing same-sitting bilateral cataract surgery. It is becoming accepted practice and mainstream.
Immediately sequential bilateral cataract surgery (ISBCS) involves performing phacoemulsification with intraocular lens implantation in both the eyes of a patient, sequentially in the same operative sitting. There are well-documented advantages in terms of quicker visual rehabilitation and reduced costs. The risk of bilateral simultaneous endophthalmitis and bilateral blindness is now recognised to be minuscule with the advent of intracameral antibiotics and modern management of endophthalmitis. Refractive surprises are rare for normal eyes and with the use of optical biometry.
As a result of the COVID-19 pandemic, there is a large backlog of deferred patients requiring cataract surgery and I wonder whether this has driven the increasing number of units undertaking ISBCS. With regards to logistics, surgical timings and minimising number of visits to the hospital, and thus risk of exposure to COVID, there are clear benefits. Clearly, the consent process is vital and patients should be aware of the vanishingly small, but still material, risk of bilateral visual loss.
There was a 50:50 split regarding consent for both eyes at the same time. While I appreciate that the risks and benefits are typically exactly the same, there are nuances which may be different between the two eyes. I do not think that cataract surgery is a procedure that should be consented for as if it were a course of treatments, unlike intravitreal injections for example.
When the patient has blurred vision in both eyes they need visual rehabilitation, so their attitude to risk may be different. Once they are achieving 6/6 in their first operated eye their position and attitude to risk may be different for their 6/12 second eye, which really does not trouble them. Furthermore, the patient who has had one eye done and it all went well is different in attitude to the same patient who was surgery naïve.
This is a positive, as they have already experienced the procedure and know intimately what to expect. However, on the negative side they often believe that nothing can go wrong, and it is a straightforward undertaking with no risk. This is clearly not the case. I always explain to my patients that the risks involved in their second eye surgery are the same as for the first eye and just because they sailed through the first eye, it does not necessarily mean that they will sail through the second eye.
The next question referred to the local restrictions on NHS cataract surgery. I have local restrictions imposed upon my NHS practice for cataract surgery and it is always very disappointing and upsetting to have to turn poor patients away. With two thirds of us not having restrictions while a third do it seems an unfair postcode lottery. When restrictions are in place, it seems the majority are based on visual acuity.
The National Institute of Health & Care Excellence (NICE) Guidance on cataract surgery states:
“1.2.2 Do not restrict access to cataract surgery on the basis of visual acuity, and 1.6.2 Offer second-eye cataract surgery using the same criteria as for the first-eye surgery (see referral for cataract surgery)” [1].
It seems unfair that some patients are restricted and others not, particularly as it seems counter to the published NICE Guidance.
There also seems to be a difference in which level of visual acuity renders the patient eligible for second eye surgery, with a third having a target set at 6/12 while more than half must have their patients 6/18 or worse in their second eye to be able to offer them NHS cataract surgery.
The next question relates to the use of the electronic patient record (EPR). Two thirds of respondents use it and I do think it is the way of the future. There are some downsides, however. Tick boxes are useful and can assist in data collection, however, the failure to tick a box or register a response can be deemed to be evidence that you did not undertake a certain step. Failure to put anything in the cornea examination box could be deemed to be evidence that you failed to examine the cornea and that the subsequent problems with postoperative corneal oedema could be attributed to your failure to examine the cornea and pick up the corneal guttatae. Try to be thorough with your data input so it can be demonstrated later that an appropriate examination was undertaken.
The last two questions touch on a subject we have discussed previously, which is the biometry check prior to surgery. With two thirds of you using the EPR it was interesting to assess whether you still utilised paper biometry. The majority of respondents still use a paper biometry, which I prefer in my practice. Being able to circle and sign the biometry is invaluable and helps the preoperative checks. Until EPRs are properly able to allow us to pick, highlight, check and double-check lens powers then I think the old-fashioned paper print out still has its place. It can still be scanned into the EPR in any case once the procedure is finished.
I was delighted to see that the vast majority of respondents double-check the biometry against the patient details, and I believe this is vital. It is a simple check and takes moments.
Once more we have achieved some useful insights into how we practise and how we do things differently. We need to act in an evidence-based way and be able to demonstrate that the safety of our patients is at the heart of everything we do.
I am grateful to all the clinicians who took time to respond and would encourage you to email me with questions you would like answered.
Reference
1. NICE Cataracts in adults: management [NG77]. The National Institute for Health and Care Excellence.
www.nice.org.uk/guidance/ng77
Last accessed March 2022.
COMMENTS ARE WELCOME






