The rise of syphilis transmission rates over the past two decades has been one of public health’s great puzzles. In the UK, the situation has reached epidemic levels, with a 126% increase between 2013 and 2018 [1]. We present a case report of optic neuropathy and choroiditis secondary to primary syphilis. This is an unusual first presentation and not an established pattern of syphilitic ocular manifestation. The diagnosis was established by a full infective screen allowing for timely and appropriate treatment.
Case report
A 46-year-old type one diabetic male with a background of pre-proliferative diabetic retinopathy (R2M0P1) in both eyes presented to the ophthalmology emergency clinic reporting a four-day history of painless, progressive loss of vision in the left eye (LE). He described a unilateral curtain-like obscuration of left vision, worst centrally.
His right eye (RE) was unaffected. Best corrected visual acuity (BCVA) was 6/120 LE and 6/9 RE. Pupils were equal and reactive to light (PERLA) with no relative afferent pupillary defect (RAPD) detected. Intraocular pressures (IOP) were within normal limits. Fundal examination identified left optic nerve swelling with left peripheral superotemporal retinal pigmentation and vascular tortuosity. There were no signs of proliferative diabetic retinopathy in either eye. Optical coherence tomography (OCT) imaging demonstrated bilateral retinal pigment epithelium (RPE) irregularities, worse in the LE compared to the RE, with mild associated photoreceptor disturbance. In the LE, fundus fluorescein angiography (FFA) showed delayed ocular perfusion, patchy choroidal filling with poor perfusion temporally, and late leakage from the optic disc. The RPE had a mottled appearance in both eyes.
The working diagnosis was left optic neuropathy and bilateral choroiditis. Figure 1 summarises all retinal imaging modalities.
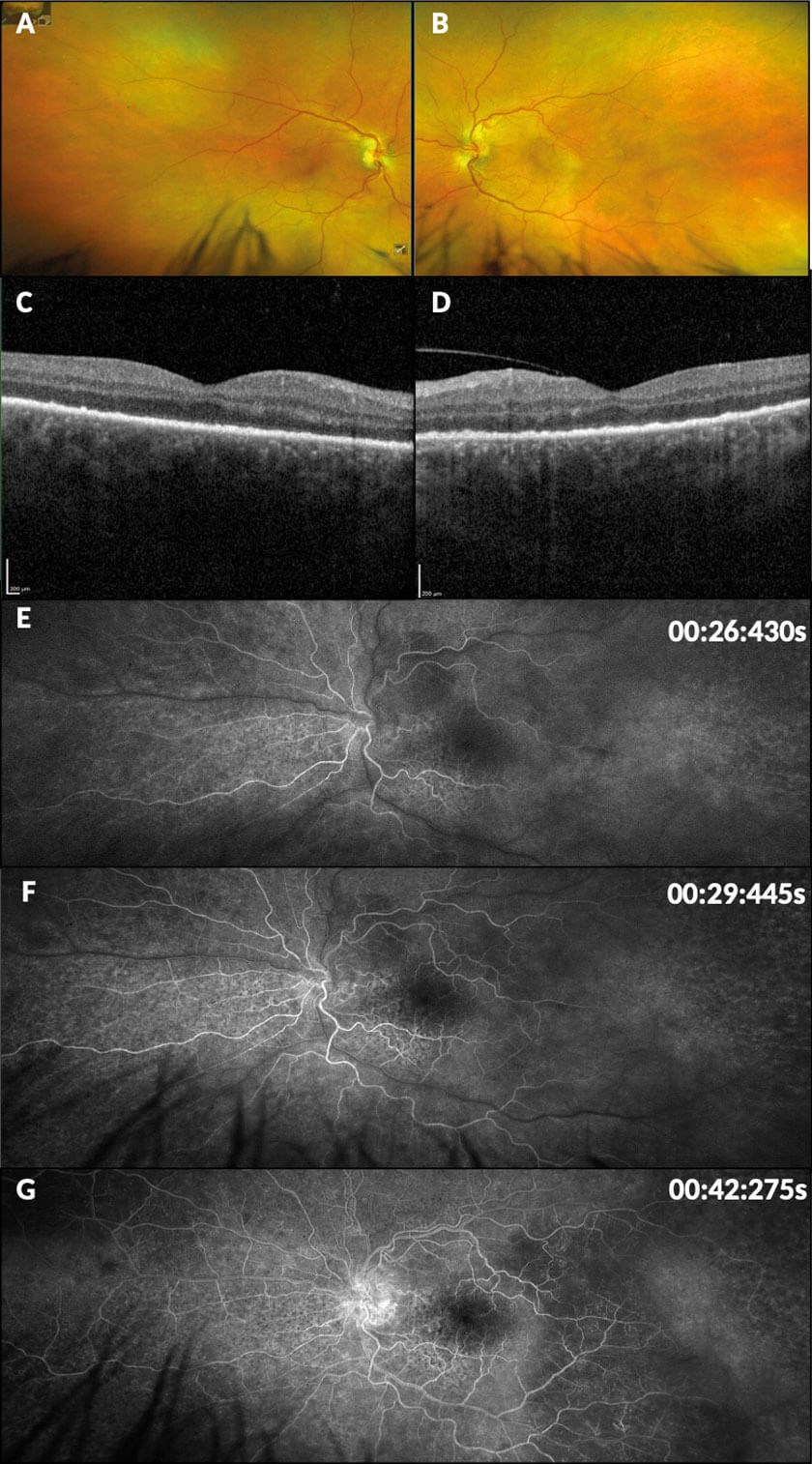
Figure 1: Retinal imaging modalities. A-B Optos colour fundus photographs: (a) right eye showing hard exudate at the periphery of the superotemporal arcade; (b) left eye showing indistinct disc margins, RPE irregularities and depigmentation at the periphery of the superotemporal arcade, a blot haemorrhage and ghost vessel far distally to the inferotemporal arcade. C-D Ocular coherence tomography: (c) right eye showing minor RPE irregularity; (d) left eye showing marked hyperreflective nodulatity of the RPE with loss of photoreceptor inner segment / outer segment layer architecture. E-G Left eye fundus fluorescein angiography with timestamps: (e) early arterial phase showing late perfusion; (f) early venous phase with marked nasal RPE mottling; (g) late venous phase demonstrating delayed perfusion, disc leakage and watershed choroidal filling defect temporally.
Subsequent assessment showed total absence of colour vision in the LE with Ishihara colour plates and normal colour vision in the RE. 30-2 Humphrey visual fields were performed, demonstrating a generalised LE visual field deficit and patchy superotemporal and inferonasal RE defects (see Figure 2).
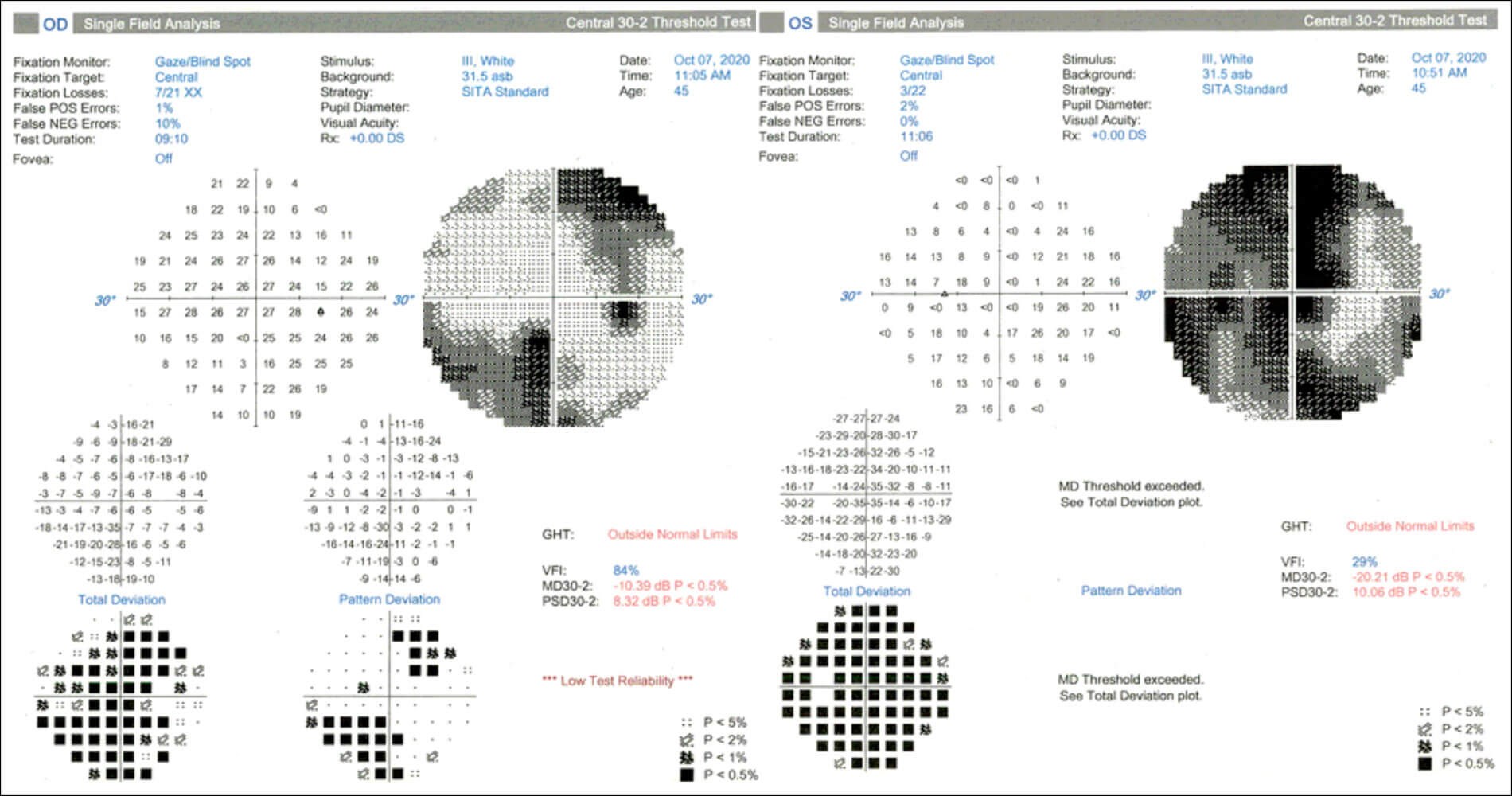
Figure 2: 30-2 Humphrey visual fields. Right eye demonstrates patchy defects superotemporally
and inferonasaly. Left eye demonstrates diffuse reduction in visual field.
The patient had soft pulsatile temporal arteries. Pertinent negatives in the history included the absence of headache, jaw claudication and scalp tenderness. Due to the findings of left optic disc swelling and mildly raised inflammatory markers (CRP=22, ESR=50) on initial blood screen, acute anterior ischaemic optic neuropathy (AION) secondary to giant cell arteritis (GCA) was suspected. Following discussion with rheumatology, a temporal artery biopsy (TAB) was planned and the patient was commenced on 40mg oral prednisolone once daily in view of this.
However, given the atypical GCA history, only mildly elevated inflammatory markers and unexplained bilateral choroiditis, a full autoimmune and infective screen was sent to exclude other causes of non-ischemic optic neuropathy (NAION) and choroiditis. This included: antinuclear antibodies, anti-neutrophil cytoplasm antibodies, rheumatoid factor, thyroid function tests, Lupus anticoagulant, anti-cardolipin antibody, anti-beta-2 glycoprotein, hepatitis screen, HIV antibody screen and syphilis serology (VRDL, RPR and TPPA). From this screen, the VDRL and TPPA returned positive, with an RPR of 1:64 indicating an acute syphilis infection. HIV serology and other screening tests were negative. A final diagnosis of syphilis-related optic neuropathy and choroiditis was made.
"In the UK, there is no screening programme for syphilis beyond antenatal testing to prevent maternal transmission. In other words, the epidemiological group with the highest syphilis prevalence and incidence rates is not screened."
Following these results, the patient was called back for urgent review, at which point his BCVA had deteriorated further to hand movement (HM) LE and 6/24 RE, with total absence of colour vision bilaterally. Fine bilateral inferior keratic precipitates and bilateral anterior chamber (AC) flare with 0.5+ cells was newly observed, with no vitritis. His right disc had become moderately elevated and the left remained swollen. There was also new RE patchy peripheral retinal pigmentation noted.
The patient was admitted under the infectious diseases team. On general examination, there were no neurological deficits and no genital lesions. A painless ulcer on the roof of the mouth was identified and diagnosed as a syphilitic chancre. A detailed sexual history revealed several occasions of unprotected male-to-male intercourse within preceding months.
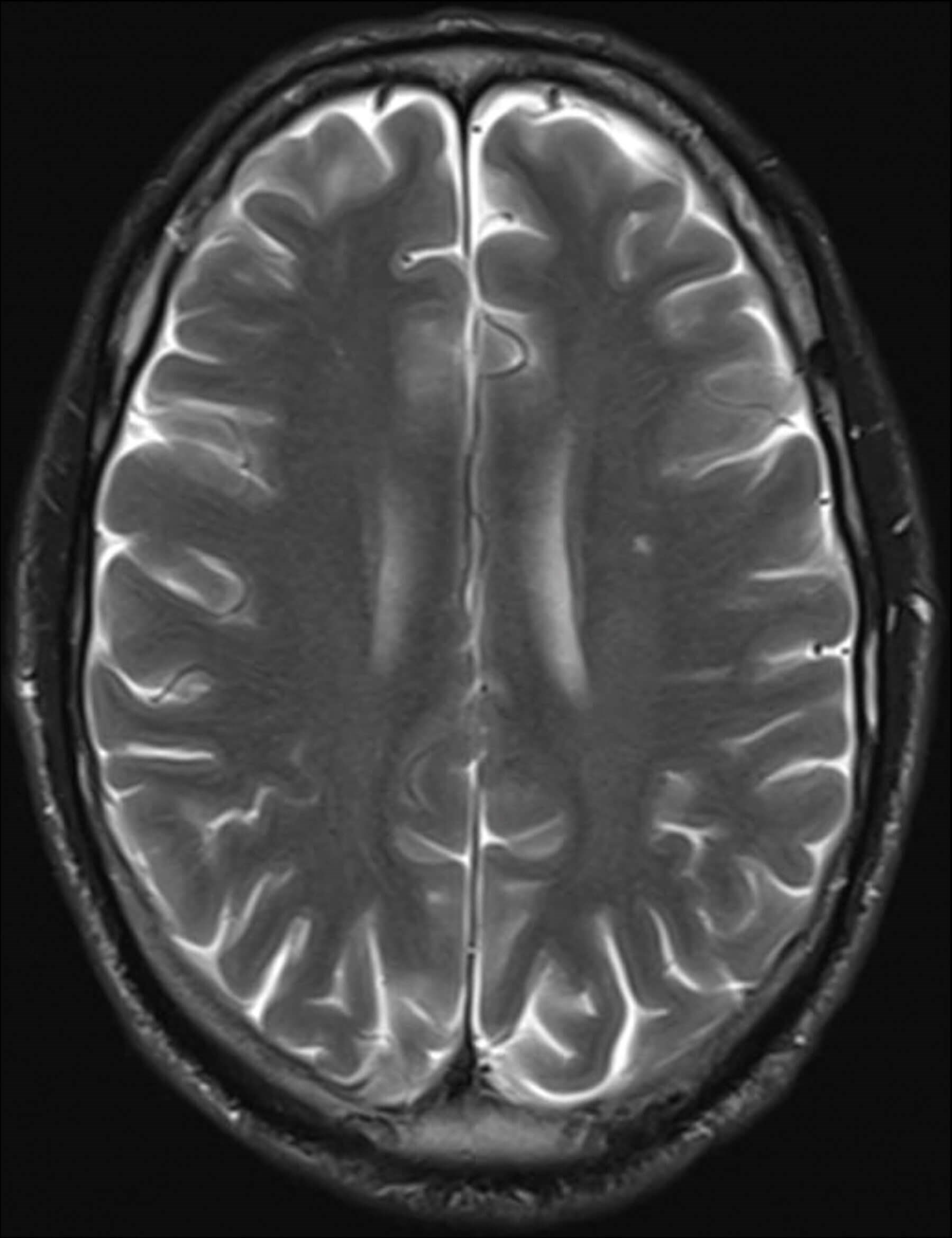
Figure 3: Contrast magnetic resonance imaging. Small nonspecific focus of hyperintensity on T2 and FLAIR sequences within the left centrum semiovale, and mild dural thickening and enhancement overlying the cerebral hemispheres bilaterally.
Contrast magnet resonance imaging (MRI) of head and orbit (Figure 3) showed a non-specific hyperintense focus on T2 and FLAIR sequences in the left centrum semiovale, and meningeal enhancement of both hemispheres. There was no enhancement or abnormality of the optic nerves and no evidence of tertiary syphilis. Cerebrospinal fluid (CSF) obtained by lumbar puncture was positive for TPPA without RPR, likely representing transfer from peripheral circulation and not neurosyphilis.
Therapy was initiated as an inpatient, consisting of a single dose of intravenous (IV) ceftriaxone followed by course of IV benzylpenicillin (2.4mg, four times a day), together with pulsed IV methylprednisolone, 1g once daily, for three days, followed by 60mg oral prednisolone once daily, and topical dexamethasone drops to both eyes. The patient was reviewed daily by ophthalmology and discharged nine days after admission. His BCVA improved to 6/12 RE 6/18 LE, although colour vision did not return with only the test Ishihara plate seen in each eye. RPE changes resolved on OCT, with physiological cupping returning bilaterally to the optic nerve heads. Oral prednisolone was tapered by 10mg per week upon discharge. The patient was discharged from the infectious diseases ward with regular follow-up in the neuro-ophthalmology department.
Discussion
Syphilis is a sexually transmitted bacterial infection caused by the spirochete Treponema pallidum. Signs and symptoms vary depending on disease stage (primary, secondary, latent or tertiary). Multi-organ vasculitis, from perivascular lymphocytes and plasma cell infiltration, is the primary mechanism of action [2]. In the eye, vasculitis typically affects the choroidal vessels and the blood vessels supplying the optic nerve head.
Ocular syphilis most commonly manifests as posterior uveitis or panuveitis [3]. Posterior placoid chorioretinitis, when present, is considered pathognomic [4]. Optic neuropathy, the initial finding in this case, is a documented (though rarer) occurrence. Optic neuritis with no signs of uveitis is reported to occur in 40% of syphilitic eye disease patients [5] – with inflammatory disc oedema accounting for 70% of all such cases, and optic atrophy, gummata and papilloedema found in the remainder [6].
Imaging was an important component of assessment, particularly considering the absence of obviously pathological retinal features on fundoscopy. Our patient showed temporal choroidal filling defects and RPE mottling characteristic of syphilitic eye disease [7]. However, this case showed less focal hypoperfusion, particularly at the macula. This may be due to an earlier presentation and / or limited choroidal involvement.
Prompt diagnosis is essential, as ocular syphilis is reversible with treatment. Excellent visual outcome post-treatment has been reported in the presence of florid retinal vasculitis, neurosyphilis and anterior uveitis [8]. One case series of ocular syphilis demonstrated visual outcome of at least 6/12 in all 17 patients presented [9].
In the present case, there was significant improvement in visual acuity after initiating antibiotic therapy (6/12 RE, 6/18 LE from 6/60 RE, HM LE), and further improvement is expected in future. The importance of prompt diagnosis of syphilis and commencement of appropriate antibiotic therapy is a learning point, as the initial treatment with 40mg oral prednisolone only saw further deterioration of vision (6/60 RE, HM LE from 6/9 RE, 6/120 LE). Little is known regarding the prognosis of colour vision defects in syphilis – lack of early resolution for this patient suggests that his loss of colour vision is likely permanent.
The importance of screening blood tests in making a definitive diagnosis is key in this case. Without screening, the correct diagnosis would not have been established so rapidly, if at all, and the patient may well have developed significant permanent vision loss. It is estimated that 82.5% of experts routinely include syphilis serology in patients presenting with uveitis of any kind [10]. Testing rates may well be lower amongst trainee ophthalmologists (who tend to be the first to see such patients in the casualty setting) and non-specialists. Given syphilis’ wide-ranging presentations, this may indicate a considerable under investigation and subsequent failure to initiate curative treatment.
Data from Public Health England shows that men who have sex with men (MSM) are the largest group diagnosed with syphilis, comprising 75% of all diagnoses (the majority of whom have an unknown or negative HIV status) [1]. Other risk factors for syphilis include positive HIV status, drug abuse, multiple simultaneous partners and unprotected sexual intercourse [11]. In the UK, there is no screening programme for syphilis beyond antenatal testing to prevent maternal transmission. In other words, the epidemiological group with the highest syphilis prevalence and incidence rates is not screened. Currently detection of syphilis in MSM rests largely with individuals themselves understanding their own risk and accessing testing via sexual health services. Given that syphilis meets the Wilson-Jungner screening criteria, and considering the social and cultural marginalisation of MSM, there is a strong argument to be made for implementation of a national syphilis screening programme for those most affected.
Conclusion
In cases of optic neuropathy and choroiditis, it is vital to rule out associated systemic pathology. Whilst posterior uveitis is the most common ocular manifestation of syphilis, this notorious great mimicker can often present atypically. A high index of suspicion for syphilis is crucial in instances of diagnostic uncertainty. As this case demonstrates, a full autoimmune and infective screen may be the only way to establish a correct diagnosis and thereby commence appropriate treatment. The Canadian Physician Sir William Osler once famously said that “he who knows syphilis knows medicine.” Perhaps, the truism for our time is that those who know medicine remember to screen for syphilis.
TAKE HOME MESSAGES
-
A high index of suspicion for syphilis is crucial in cases of diagnostic uncertainty.
-
A full autoimmune and infective screen can establish a correct diagnosis and treatment pathway.
-
MSM are the largest epidemiological group diagnosed with syphilis (75%). Other risk factors for syphilis include: positive HIV status, drug abuse, multiple simultaneous partners and unprotected sexual intercourse.
-
Ocular syphilis most commonly manifests as posterior uveitis or panuveitis.
-
Ocular syphilis is amenable and highly responsive to treatment.
References
1. Public Health England. Addressing the increase in syphilis in England: PHE Action Plan June 2019.
https://assets.publishing.service.gov.uk/
government/uploads/system/uploads/
attachment_data/file/806076/Addressing
_the_increase_in_syphilis
_in_England_Action_Plan_June_2019.pdf
2. Carlson JA, Dabiri G, Cribier B, Sell S. The immunopathobiology of syphilis: the manifestations and course of syphilis are determined by the level of delayed-type hypersensitivity. Am J Dermatopathol 2011;33(5):433.
3. Tsimpida M, Low LC, Posner E, et al. Acute syphilitic posterior placoid chorioretinitis in late latent syphilis. Int J STD AIDS 2009; 20(3):207-8.
4. Gass JD, Braunstein RA, Chenoweth RG. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology 1990;97:1288-97.
5. Northey LC, Skalicky SE, Gurbaxani A, McCluskey PJ. Syphilitic uveitis and optic neuritis in Sydney, Australia. Br J Ophthalmol 2015;99(9):1215-19.
6. Klein A, Fischer N, Goldstein M, et al. The great imitator on the rise: ocular and optic nerve manifestations in patients with newly diagnosed syphilis. Acta Ophthalmol 2019;97(4):e641-7.
7. Burkholder BM, Leung TG, Ostheimer TA, et al. Spectral domain optical coherence tomography findings in acute syphilitic posterior placoid chorioretinitis. J Ophthalmic Inflamm Infect 2014;4(1):2.
8. Balaskas K, Sergentanis TN, Giulieri S, Guex-Crosier Y. Analysis of significant factors influencing visual acuity in ocular syphilis. Br J Ophthalmol 2011;95(11):1568-7.
9. Hughes EH, Guzowski M, Simunovic MP, et al. Syphilitic retinitis and uveitis in HIV‐positive adults. Clin Exp Ophthalmol 2010;38(9):851-6.
10. Oliver GF, Stathis RM, Furtado JM, et al. Current ophthalmology practice patterns for syphilitic uveitis. Br J Ophthalmol 2019;103(11):1645-9.
11. Solomon MM, Mayer KH. Evolution of the syphilis epidemic among men who have sex with men. Sex Health 2015;12(2):96-102.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME





