
Despite the help of allied health professionals in triaging and managing acute ophthalmic emergencies, eye casualty remains overburdened. Trainees at the beginning of their training often struggle to manage such busy clinics with varied presentations.
We present a case that presented as a retinal detachment as per the patient’s own perception but was diagnosed correctly in casualty after extensive history and examination. A careful history conducted at the start of the consultation may have resulted in a more focused examination and early diagnosis, thereby saving the trainee time in a busy clinic.
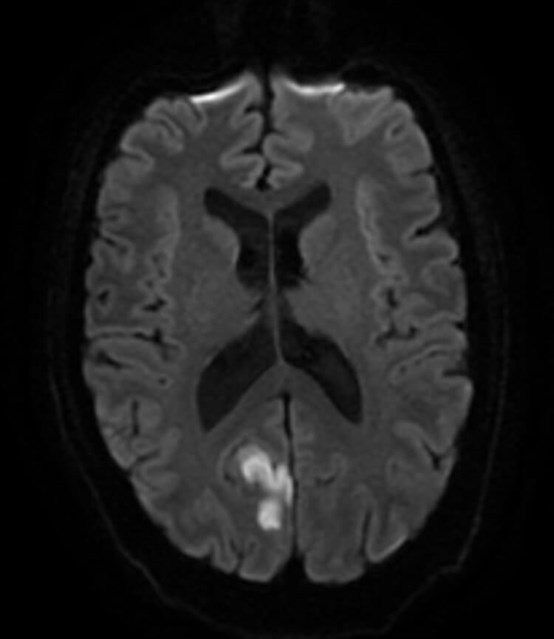
Figure 1: MRI head showing right occipital lesion infarct that produced the left inferior homonymous quadrantopia.
Case report
A 60-year-old gentleman with A family history of retinal detachments presented with loss of vision in the inferior temporal visual field of his left eye. The patient first noticed symptoms the same day at 4am but denied any other visual symptoms. The patient was referred by the GP practice for urgent review due to suspected retinal detachment. The patient was seen in eye casualty the same day.
On further probing of the history the patient revealed that he had had a right haemorrhagic PVD 10 years previously. There was no other family history of significance, and past medical history was significant for the absence of cardiovascular risk factors.
The patient was extremely concerned for a retinal detachment given his extensive family history. Vision was 6/6 bilaterally. Slit lamp examination revealed an unremarkable anterior segment bilaterally. Vitreous examination initially showed no pigment, with a PVD present in both eyes. A dilated fundal examination with 90D lens and scleral indentation with indirect ophthalmoscope failed to reveal any retinal tears or retinal detachments.
The patient’s visual fields were examined using gross confrontational field testing. The examination revealed bilateral loss of vision in the left inferior nasal quadrant. It was deemed that the patient was more likely to have had a stroke with a left inferior quadrantanopia as the cause of his symptoms. The stroke team was informed, and a full work up was carried out.
A stroke team assessment gave the patient a NIHSS score of 1. A CT head and a MRI head was ordered. The CT head showed an extremely subtle decreased density in the right occipital lobe which was suggestive of a sub-acute infarct. MRI DWI imaging confirmed the lesion. Based on the above workup, the diagnosis was confirmed as sub-acute right occipital infarct which was the cause of the left homonymous inferior quadrantanopia field defect.
Comments
The case highlights some key learning points. Firstly, whilst due consideration must be given to the patient’s self-diagnosis, the clinician should strive to arrive at the diagnosis independently. The initial history was indicative for a left eye superior nasal detachment. However, many patients with bilateral homonymous field defects do not notice their visual defects bilaterally, which leads to GPs referring the patients to ophthalmology.
Secondly, a thorough history must be taken, and in this instance, questions specifically asking if any previous posterior vitreous detachment events occurred in the left eye or asking him to specifically check if the field defect was monocular would have been extremely helpful. In the same vein of thought, a thorough examination with a confrontational visual field test at the start of the examination could have been considered.
Although it is classically taught in medical school that quadrantopias localise to the parietal lobe (inferior quadrantopia) or temporal lobe (superior quadrantopia), specific field defects do not always point a specific lesion location. A recent study actually showed that 76% of lesions that cause inferior quadrantopias were found in the occipital lobe, whilst only 22% were isolated to the parietal lobe [1]. Lesions must be confirmed with neuroimaging, and in the case presented above, MRI DWI imaging showed a right occipital infarct as the cause of the left inferior quadrantopia (Figure 1).
Another way clinicians can isolate lesion locations is by documenting any associated symptoms. Aphasia of the parietal lobe (specifically conduction aphasias) are associated with lesions of the left deep parietal lobe. Whilst left sided neglect is the most common right parietal lobe lesion associated with strokes [2], lesions in the parietal lobe may be associated with other localising lesions.
Often the patient’s primary concern after being informed of the diagnosis will be treatment and recovery period. Whilst it must be stressed that most treatment moving forward will be for the prevention of further related symptoms including large strokes, there can be around 50% improvement in the lesion itself. However, if any improvement is to take place this usually takes place within the first three to six months of the primary event and improvement thereafter is minimal [3].
Medical management of cerebrovascular accidents (CVA)
- Cerebrovascular accidents is an umbrella term incorporating both strokes and transient ischaemic attack (TIA).
- CVAs are either ischaemic or haemorrhagic in origin, with 70% of strokes being ischaemic in origin. In contrast, TIAs are overwhelmingly ischaemic in origin, with only a small subset of patients on anticoagulants being at increased risk of haemorrhagic TIAs.
- TIAs are usually treated with high dose aspirin 300mg once a day for two weeks, with 75mg of clopidogrel once a day lifelong thereafter. However, if the patient is on anticoagulants the patient must undergo investigation with a CT head scan to exclude haemorrhagic TIA before administering aspirin. A referral to the stroke team is essential, with a review preferable within a week.
- Patients with stroke will have similar treatment but will all undergo head CT scans before any treatment decisions are made to rule out haemorrhagic pathology. Haemorrhagic strokes have good prognosis and are usually treated conservatively unless there is a neurosurgical indication.
- Ischaemic strokes may be treated with thrombolysis if indicated. Increasingly a small number of UK centres have started to offer thrombectomy. Patients who do not undergo either of these procedures are under the regular standard treatment of two weeks of high dose aspirin followed by 75mg of clopidogrel lifelong for secondary prevention. Physiotherapy remains the mainstay of treatment for patients with severe strokes.
- Patients will undergo investigations aiming to identify the aetiology of stroke to prevent future CVA events.
References
1. Jacobson DM. The localizing value of a quadrantanopia. Arch Neurol 1997;54(4):401-4.
2. Sinanović O. Neuropsychology of acute stroke. Psychiatr Danub 2010;22(2):278-81.
3. Rowe FJ, Wright D, Brand D, et al. A prospective profile of visual field loss following stroke: prevalence, type, rehabilitation, and outcome. Biomed Res Int 2013;2013:719096.
COMMENTS ARE WELCOME





