Ocular motility can often be a slightly abstract concept during the earlier years of ophthalmology training. A large variance on what embodies normality; mythical concepts like fusion and binocular vision, examination techniques that can be fiddly, and complex neuroanatomy all conspire to make it an awkward topic to learn.
The concepts that are more pertinent to general training relate to the diagnosis and management of pathologies that will lead to strabismus and / or diplopia.
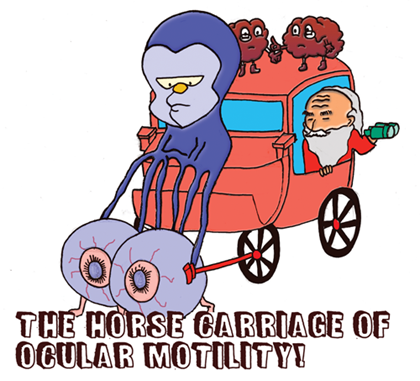
Figure 1: A caricature of ocular motility (Illustration by Shindy Je).
Basic control of eye movements
In our oversimplified analogy, the brain stem is a complex guy as you can tell from his expression in Figure 1. He grew up in a complex environment with complex relationships and apart from driving the movement of the eyes is also responsible for a multitude of vital basal functions. He is a skilled driver of the eyes and has honed these skills through years of inherited and acquired learning. Inside his body there exists an intricate interweaving body of connections that make him function so well (textbooks have been written on his complexity). All eye movement, whether calibrated by the navigator in the back seat (cerebellum) or voluntarily directed by the little lobes of brain at the top (frontal eye field) will have to be performed by our chauffeur, the brainstem.
The eyes work best as a pair. If humans had only one eye by design, parts of our brainstem would probably be more rudimentary (and doing a cover test will look very silly) but having two opens up a whole world of motor and sensory function.
To stabilise the eyes, a constant signal is sent in order to keep them relatively in the correct position. If both eyes can individually see well the brain can coordinate both foveas to fixate on the required target. When we disassociate the eyes, i.e. an alternate cover test, we halt that process and the eyes return to that ‘resting position’, hence we are able to see the latent squint or a phoria.
Think about a manifest squint in an amblyopic exotropic eye. Due to suppression of the image coming from one eye, the brain has lost the ability to coordinate both eyes at the same time. Hence, the (usually poorer seeing) eye drifts to a ‘resting position’, the good eye fixates on the target, and you see a manifest squint or a tropia.
Often the science makes sense, an accommodative esotropia occurs because the accommodation effort to overcome the hypermetropic blur causes an overconvergence. Occasionally though, through mechanisms that are not completely understood, the dynamics of the characters in our story are strained and the final message sent to the eyes is mixed, resulting in non-alignment.
In a child, when a motility problem leads to diplopia / confusion, the brain really dislikes it as you can imagine, and is forced to suppress one image in order to be of any use to society. It can also be the other way around where the vision is affected first and the brain no longer has a pair of good images that it can use in order to develop precise coordination. It then could partially switch off depending on its mood and may just leave things be to the ‘resting tone’ or tweak a little here and there occasionally.
Therefore, this resting tone, although there are default settings that come with a new brainstem, is subject to change during development, can vary slightly over time and within individuals, and can be occasionally swayed by pathology.
As human beings when we get older or more tired, we decompensate in many areas unfortunately. The fusional vergence system is subject to this as well. When it breaks down, the eyes will drift to its resting position but because we are not covering either eye, the foveas are not in sync and we see double. A decompensating heterophoria is the most common cause for an intermittent diplopia.
Being very visual beings, we depend a lot on our vision to orientate us on this plane as well as to track objects of interest, either when making a bifoveal smooth pursuit of a rabbit scurrying across the forest floor, or a patient’s quick saccades around the operating room as he is lying on the operating table trying to determine if you or the consultant will do his cataract.

Figure 2: Cartoon of a confused caveman.
Horizontal strabismus is more common, because we have complex vergence mechanisms that function to converge and diverge the eyes allowing us to focus on objects along the same plane so there are more things that can ‘go wrong’ during the development of binocular vision. Why horizontal? Because our eyes are placed side by side and not on top of one another (Figure 2).
What about vertically? The basic role of the vertical centres is to make sure that our set of horizontally placed eyes stay level in relation to each other, as well as adapting to the earth’s vertical line. Without these mechanisms, we will be fuddled with the slightest of head movements.
The players
The frontal cortex on each side initiates a conjugate saccadic process to the contralateral side. This starts the saccadic pathway which travels down to the superior colliculus. To aid in remembering, if you refer to our lovely drawing, you can see that the characters stood on top of the carriage are pointing to the other side. An agitated lobe (i.e. an irritative lesion like epilepsy) will be more demanding, make a bit more noise, and this will cause the driver to move in that direction. If the lobe is quiet (i.e. destructive lesions like a stroke), his opposite partner will take over and the eyes will move to the affected side.
The cerebropontocerebellar pathway, AKA pursuit pathway (wheels of the carriage), maintains smooth pursuit of an object while optical feedback is constantly being regulated by the cerebellum (wise old man with binoculars) so that the movement is at the right velocity (if the speed and direction of where the eyes should go next are not determined, we will be useless at fixating on a moving object). Cerebellar disease is a common cause of nystagmus.
All these signals communicate with one another via interconnecting neurons in order to generate a message that tells the brainstem where to go, how fast to get there, and when to stop.
The brainstem with this information then directs the eye movements via impulses sent through the third, fourth and sixth nerve on both sides. As he is a clever little chap himself (even receiving sensory input directly from retinal ganglion cells), he makes little decisions in his supranuclear centres before deciding how to direct his reins to do horizontal or vertical manoeuvres and when to converge or diverge depending on the type of movement he has been told to make.
Things that can go wrong
We have already discussed developmental features but what about acquired disease?
Let’s take our analogy and work our way from front to back. It is natural to note that as we go further backwards, it gets a little less familiar and the words become fancier.
The eyes need to travel as a pair so a mechanical defect affecting one eye or both will impair the movement of the eyes (orbital / globe pathology). Examining the eyes is what we are good at so this is our comfort zone.
The reins of the brainstem (cranial nerve pathology) can be affected partially or fully, isolated or in combination and this will result in the eye or eyes not being able to make specific movements. This is the infranuclear pathway and we can usually relate better to pathologies in this area.
The brainstem. Here we can have pathology affecting the nucleus of the reins, the connections between the cranial nerves (the medial longitudinal fasciculus), or the supranuclear gaze control centres. A host of other cranial nerves and other important structures (like the bundles of nerve between brain and spinal cord) travel within the brainstem so other neurology can easily coexist (and should not be missed).
As we enter supra-brainstem territory, it gets more complex but generally we have the saccadic pathway and the pursuit pathway which is initiated and regulated separately but recent evidence suggests they work a lot closer together than once thought.
Our role as ophthalmologists
With our understanding of the visual system, we should be equipped to do the following:
Diagnosis: Localising the disease
By working through what governs motility, we can work our way from an inferior orbital floor fracture leading to failure in unilateral upgaze and vertical diplopia. Or a cerebellarpontine angle tumour leading to a mixed craniopathy and nystagmus. There is merit in localising well as we could potentially diagnose life-threatening disease.
It is not uncommon for this caseload of patients to present to the ophthalmology team first.
Management
Once we know the aetiology, we can:
- Treat the underlying cause. This could range from fixing the refractive error to treating orbital inflammatory disease medically to repairing a muscle avulsion.
- Treat amblyopia if it exists. Patching is a wonderfully rudimental treatment that has survived the test of time.
- Maintain alignment. Generally, once things are stable, we are able to improve vision or improve cosmesis by manually strengthening or weakening individual muscles.
Quick examination of patients for exam purposes
In an exam setting, it makes sense to have a methodology which is comprehensive and includes all aspects of motility. However, one should be careful not to do too many unnecessary steps. This system is designed to pick up the likely diagnosis as soon as possible in order for you to decide on which subsequent examination to use next. Keep in mind that as soon as you recognise the diagnosis, you have to modify the rest of your examination accordingly. For example, if you spot a prosthetic eye from the moment you see the patient, you don’t want to waste any time getting them to fish their elusive spectacles out of the coat pocket so you can do a near and distance cover test with and without their spectacles. Conversely, those steps might be the most important ones for conditions like a distance esotropia or a fully accommodative esotropia so make sure you consider them in those scenarios.
An impression of being ‘slick’ comes not from doing things very quickly but rather from doing the required steps correctly the first time around.
“In an exam situation we are expected to come up with a diagnosis based on our three minute motility examination.”
Unlike real life, where we have the benefit of doing something devious called taking a history, in an exam situation we are expected to come up with a diagnosis based on our three minute motility examination with usually only a little background of the underlying problem.
Start off looking for the obvious –
Head Posture, Eyelids, Aperture (pupils), Deviation (H.E.A.D)
This is the inspection phase. It is not exhaustive but each feature in the acronym is crucial because if present it may very well lend itself to a spot diagnosis!
If they are normal, it only takes 5.3 seconds to say: “This patient has no abnormal Head tilt, normal Eyelids with no obvious asymmetry, no abnormalities with the pupil Apertures, and no Deviation on primary gaze.”
Even before you actually start, you would have considered a myriad of conditions. Example:
- Head Posture: face turn – sixth nerve palsy, head tilt – fourth nerve palsy, chin depression – bilateral fourth nerve palsy, chin elevation – chronic progressive external ophthalmoplegia (CPEO).
- Eyelids: unilateral ptosis – Horner’s / third nerve / trauma / myasthenia, bilateral ptosis – CPEO, myasthenia, lid retraction – thyroid disease, contralateral ptosis, enophthalmos – enucleation socket syndrome, proptosis – orbital / cavernous sinus disease.
- Aperture: Anisocoria – Horner’s / third nerve, mid-dilated pupils – parinauds, constricted pupils – convergence spasm.
- Deviation: nystagmus, internuclear ophthalmoplegia, wall-eyed bilateral internuclear ophthalmoplegia (WEBINO), esotropias, exotropias, skew deviation, hypertropia, cranial nerve palsies, mechanical entrapment, axial and nonaxial proptosis.
If you make a spot diagnosis after the H.E.A.D phase, you can do a little wry smile because the game is over (but don’t make that smile too awkward). If you see a down and out eye with a blown pupil and a ptosis, you can mention it immediately and then cater the rest of your examination accordingly. So in the example of a third nerve palsy, do the necessary eye movements then find out if it is complete or partial, isolated or mixed, nuclear or peripheral (Oxford Handbook Third Edition page 700) and so on.
NB: When you see a third, fourth or sixth cranial nerve palsy at any stage, make sure you test (or at least mention it) for all the other cranial nerves (especially from second to eighth).
The Ophthalmology Examinations Review by Wong et al. has excellent clinical approaches to different motility conditions.
STEP ONE: Primary position (diplopia / pupils / cover test)
- Ask patient: “Do you have any double vision?”
The presence or absence of diplopia (and its features: horizontal, vertical, tilted) in either the primary position or other positions will help narrow down the condition. - Hirschberg Test to recheck primary deviation.
- Cover Test (if you do it properly first time you only need to cover each eye ONCE) distance then near.
- Alternate Cover Test (again, do it properly the first time if possible). Testing with spectacles may not be necessary if they have a high prescription and can’t fixate well without the aid of their glasses.
STEP TWO: Horizontal gaze (dextroversion / laevoversion)
- Tell patient: “Let me know if you see double.”
- Move the eyes across the horizontal gazes. Once to the left and once to the right. This one move volunteers a lot of information like an overaction / underaction, upshots / downshoots, impaired / increased velocity, impaired pursuit, i.e. showing small saccades instead, or even a gaze-evoked nystagmus. This step is crucial. As a lot of pathologies affect horizontal movement, they will reveal themselves here!
- If the patient sees double, stop there and ask them to describe the nature of the diplopia and then cover each eye asking them which image disappears. The more outwardly placed image is being seen by the paretic eye. If the cover is already there, do an alternate cover test to have an idea of the size of the deviation in that position.
- If there is underaction at any stage, try to see if duction = version or otherwise.
- Orbital
– isolated horizontal muscle failure / weakness / entrapment. - Cranial nerves
– sixth nerve palsy showing ipsilateral underaction in abduction
– fourth nerve palsy showing ipsilateral hypertropia in adduction
– third nerve palsy showing ipsilateral underaction in adduction (potentially in other directions as well). - Myogenic
– Ocular Myasthenia Gravis
– CPEO. - Supranuclear / internuclear
– skew deviation (hypertropia on abduction)
– INO and WEBINO
– one and a half syndrome
– horizontal gaze palsy
– brainstem pathology
– nystagmus.
STEP THREE: Vertical gaze
- Tell patient: “Let me know if you see double.” Same principles apply:
if they see double, ask them to describe it and do a cover test to find the paretic eye. - Straight upgaze.
- Straight downgaze (lift the lids up +- elevate the chin).
- Concentrate on the four oblique movements. This will allow you to test the elevators and depressors at its position of optimal function. It is easier at this stage to think in terms of individual muscle action.
- Orbital
– thyroid eye disease
– isolated muscle failure / weakness / entrapment
– age-related upgaze weakness
– monocular elevation deficit. - Cranial nerves
– sixth nerve palsy showing ipsilateral underaction in upgaze and downgaze in abduction
– fourth nerve palsy showing ipsilateral hypertropia in adduction and inferior oblique overaction or superior oblique underaction in the direction of that muscle’s action
– third nerve palsy showing ipsilateral underaction on elevation and adduction (potentially in order directions as well). - Myogenic / neurogenic
– CPEO
– Ocular Myasthenia Gravis. - Supranuclear
– progressive supranuclear palsy
– Parkinson’s
– upbeat and downbeat nystagmus
– gaze palsy
– brainstem pathology.
Other tests (three step test, saccades, convergence, doll’s head, optokinetic drum)
These tests are used to supplement what you are already suspecting. There will not be a condition where you have to use all of them on the same patient!
If we look at our differentials, you will see that at some point during your examination, something should show up, and 50% of them will potentially have an obvious sign (hence why these patients were recruited for the exam). If you’ve done the steps correctly and everything still looks normal or the patient does not volunteer diplopia in any position of gaze, then the patient is either normal (which will be ideal in your casualty clinic but pretty much impossible in your exam) or you’ve missed something subtle but at least have demonstrated a wonderful technique.
Conclusion
Ocular motility is confusing. Most ophthalmologists don’t understand it and a portion of those have never understood it. This is a great shame as it opens the door to a beautiful interaction between eye and brain in both patient and ophthalmologist and we hope this guide above makes a difficult subject more accessible.
COMMENTS ARE WELCOME