Reactivation of varicella zoster infection in the elderly commonly presents to ophthalmologists as herpes zoster ophthalmicus (HZO), affecting the Va trigeminal dermatome.
In patients with impaired immunity, zoster infection occurs with increased severity and may be complicated by visceral and disseminated cutaneous disease [1] with atypical presentations[2]. In malignancy, particularly lymphomas, the incidence of disseminated cutaneous disease may be up to 10% in cutaneous T cell lymphoma and 9% in Hodgkin’s disease [3].
We report an uncommon clinical presentation to our ophthalmology unit which posed an initial diagnostic challenge.
Case report
An 87-year-old lady was referred to the Bristol Eye Hospital following a three day history of deteriorating right temple and periorbital swelling and pain, after minimal trauma involving a wardrobe.
Provisional diagnosis had been a secondary cellulitis at the site of trauma, which was treated with metronidazole and ceftriaxone at a local district hospital prior to referral.
There was no previous ophthalmic history of note and no ocular symptoms were reported. The patient had a 10 year history of chronic lymphocyti leukaemia (CLL).
On examination, the patient was pyrexial but otherwise systemically well. Visual acuity was 6/18 right and left (consistent with cataracts). Pupil reactions were normal, with no relative afferent pupillary defect (RAPD) and no deficit on Ishihara testing. There was no proptosis and eye movements were full.
An isolated raised plaque on the right temple at the site of trauma was noted; approximately 6cm diameter with central necrosis and ulceration and contiguous periorbital erythema and oedema of the skin (Figure 1). Ocular slit-lamp examination was unremarkable.
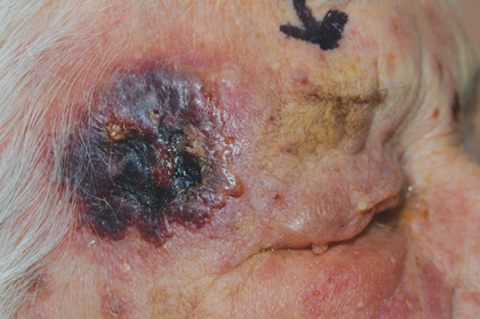
Figure 1: Right cutaneous plaque with central ulceration.
At time of presentation, white cell count was elevated 105.72 x10 ⁹/L (4 -10). Inflammatory markers were mildly elevated (CRP=9).
Multiple discrete cutaneous lesions began to develop over the face, chest, back and arms. The rash was suspected to be secondary to a drug reaction, particularly in the context of a previous allergy to penicillin (Figure 2).

Figure 2: Non-dermatomal widespread cutaneous lesions.
Urgent incision biopsy and microbiology swabs were obtained.
Histology findings were predominantly of inflammation and necrosis, with a degenerate surface squamous epithelium, representative of viral infection. Microbiology confirmed specimens were varicella zoster virus DNA PCR positive. Treatment with IV aciclovir was commenced.
The patient went on to develop blurred vision in the right eye. Right conjunctival injection, keratic precipitates and 2+ cells typical of an anterior uveitis in HZO developed, prompting treatment with topical prednisolone and cyclopentolate. Dilated fundoscopy excluded posterior involvement associated with varicella zoster infection.
New skin lesions continued to appear on the patient’s trunk – treatment was changed to valacyclovir on advice of microbiology and she has since made a good recovery.
Discussion
This case is an illustration of a common pathology presenting in an unusual way. Cutaneous leukaemic infiltrate due to CLL or fungal kerion were considered in the initial differential diagnoses.
The history of mechanical trauma triggering a localised zoster herpetic outbreak has been reported [4,5]. Reactivation may possibly be attributed to a localised disruption of cutaneous immunity and / or stimulation of the sensory nerves [6]. Depression of cell mediated immunity due to underlying CLL will have contributed to the progression to disseminated cutaneous involvement.
References
1. Ahmed AM, Brantley JS, Madkan V. Managing herpes zoster in immunocompromised patients. Herpes 2007;14(2):32-6.
2. Gnann JW Jr. Varicella-zoster virus: atypical presentations and unusual complications. J Infect Dis 2002 2015;186(Suppl 1):S91-8.
3. Vonderheid EC, van Voost Vader PC. Herpes zoster-varicella in cutaneous T-cell lymphomas. Arch Dermatology 1980;116:408-12.
4. Klauder JV. Herpes zoster appearing after trauma. JAMA 1947;134:245-8.
5. Thomas SL, Wheeler JG, Hall AJ. Case-control study of the effect of mechanical trauma on the risk of herpes zoster. BMJ 2004;328(7437):439.
6. Zhang JX, Joesoef RM, Bialek S, et al. Association of physical trauma with risk of herpes zoster among Medicare beneficiaries in the United States. J Infect Dis 2013;207(6):1007-11.
COMMENTS ARE WELCOME





