In this paper we will discuss The Rapid Assessment of Avoidable Blindness (RAAB), a survey methodology that has become the single largest source of population eye health data globally.
The origins of RAAB
The RAAB is a rapid, population-based survey methodology used to estimate the prevalence and magnitude of vision impairment (i.e. how common it is in a defined population), causes of vision impairment, and eyecare service coverage among people aged 50 years and older. The methodology was initially developed in the late 1990s to assist the planning and evaluation of district-level cataract surgery programmes in India [1]. This early version was known as the Rapid Assessment of Cataract Surgical Services (RACSS) and focussed on cataract as the most common cause of blindness.
Over time, the International Centre for Eye Health (ICEH) at the London School of Hygiene & Tropical Medicine (LSHTM) has supported the evolution of the methodology from RACSS to RAAB [2,3]. Since 2000, nearly 400 RAAB surveys have been completed globally, across 85 countries, and RAAB has become the standard methodology for generating epidemiological evidence for eye health service planning.
RAAB has evolved several times, for example to update the lowest vision testing threshold from 6/18 (RAAB5) to 6/12 (RAAB6) and developing an optional module on diabetic retinopathy. The most recent version, RAAB7, was launched in 2021 and has seen further methodological advances. This includes the addition of uncorrected distance visual acuity assessment and near vision assessment, and optional items on disability (including mental health) and socioeconomic position – each linked to higher likelihood of vision impairment through multiple pathways [4,5].
Accurate population data is crucial for health-service planning – to inform evidence-based service design and resource allocation, and to be able to set targets and evaluate progress towards these over time. Reliable local data on population eye health are imperative for countries striving to realise Universal Health Coverage (UHC), as set out by the World Health Organization (WHO) in the World Report on Vision in 2019 [6,7].
Effective cataract surgical coverage (eCSC) and effective refractive error coverage (eREC) are two population-based indicators prioritised by WHO for tracking eye health within UHC as they reflect people’s access to services and a measure of service quality. eCSC measures the proportion of people who have had cataract surgery with a good outcome (defined as a presenting visual acuity of 6/12 or better in the operated eye) out of all of those either operated on or requiring surgery, while eREC similarly measures the proportion of people in need of refractive error correction who have received it and can see at least 6/12 out of their better eye [8,9]. RAAB7 provides estimates for both, supporting countries to report against global targets for each. The optional sociodemographic variables allow eye health planners to see where underserved groups are being excluded or left behind so that they can devise approaches that better meet their needs.
Why is RAAB ‘rapid’?
RAAB is rapid for several reasons. First, it samples people 50 years and older, as the majority (around 70–80%) of blindness occurs in this age group, and therefore sample sizes are lower compared with all-age surveys [10]. Secondly, enumeration (i.e. recruiting survey participants) and examination happen on the same day, minimising field costs. Thirdly, the core examination protocol is brief. All survey participants first have their distance and near vision measured. An ophthalmologist then completes a brief lens exam on all participants and, for all participants with presenting visual acuity of less than 6/12 in either eye, assigns a main cause of vision impairment per eye and in the person. If operated or unoperated cataract is identified, several additional questions are asked. This streamlined protocol provides estimates on the prevalence and main causes of vision impairment and blindness in the population 50 years and older that are similar to an all-age survey while requiring far fewer resources [11]. Finally, since 2001, RAAB has had its own bespoke data entry and analysis software to assist users in entering data from paper forms, checking data quality and quickly generating automated results without the need for a statistician.
More recently in RAAB7, this data entry and analysis system has been rebuilt and expanded on in a collaboration between ICEH and Peek Vision, a social enterprise that develops software and data intelligence for eye health. RAAB7 uses a bespoke Android application-based data collection tool that includes Peek Acuity, a visual acuity test for mobile devices [10]. Data are encrypted to industry standards before being synced to a secure cloud-based server. As well as digitising data collection, RAAB7 includes a new web browser-based ‘Admin’ portal for users to review incoming data, quickly identify and correct errors and generate automated survey reports (see Figure 1).
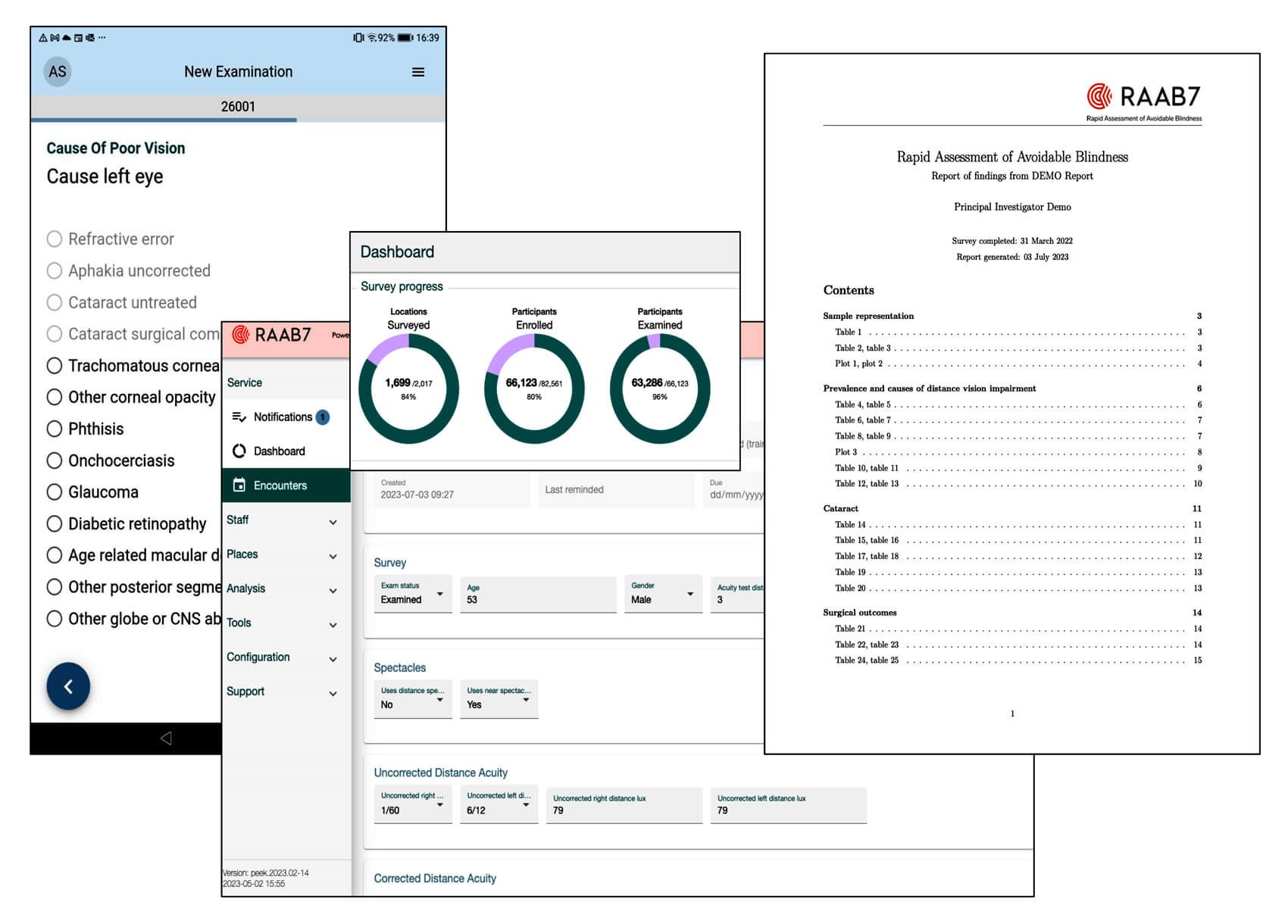
Figure 1: RAAB7 Software (dummy data).
ICEH’s role in supporting RAAB7 surveys
Building on previous iterations of RAAB, ICEH provides survey support to RAAB7 users in a number of ways. We provide template resources for writing study protocols and ethics applications, link users to RAAB trainers and provide guidance on planning for a RAAB. This includes the direct provision of technical support (for example assisting in generating sample sizes or preparing sample frames, or reviewing protocols), particularly for those requiring bespoke survey design or analysis. We also run a Training of Trainers programme for RAAB trainers, who must take an online exam and pass a structured observation before being qualified to deliver RAAB training to local teams. We make sure that trainers have access to up-to-date training resources and software guidance and provide and support to them in their role guiding users. This ensures all training is standardised and completed to a high quality and consequently that the findings are reliable for use in service planning. Standardisation also allows for comparison between settings and over time.
In 2018, we established a RAAB steering group of nominated representatives from the eye health sector, including RAAB trainers, to direct and approve further research and development of RAAB. RAAB has always provided automated survey reports to facilitate interpretation of findings. In consultation with the steering group, we reviewed the multiple reports available with RAAB6 and consolidated these into a single report of priority indicators for planning, enhanced with new outputs. We meet periodically with the steering group to propose new areas for research and development for the RAAB project to continue aligning it closely with global goals for universal eye health. In recent years, we have tested the inclusion of new socioeconomic and near vision content and are currently pilot testing new modules for health economics and health systems.
RAAB for global eye health advocacy
ICEH maintains a repository of RAAB data (www.raab.world), including information on historic RAAB data previously curated outside of ICEH. We have expanded the repository to record and report survey metadata and aim to align the repository with the FAIR principles (findable, accessible, interoperable and reusable) of research data management [12]. For example, the code for the analysis was re-written using the open source R statistical computing software and is openly available on GitHub [13]. We have also run the new RAAB7 reports for all available datasets in the repository, supporting like-for-like comparisons between older and more recent data collection.
While the primary aim of RAAB remains the provision of robust data for localised eye health planning, RAAB data are also fundamental for the global eye health data ecosystem. The Vision Loss Expert Group (VLEG) coordinate analyses of available eye health survey data for the Global Burden of Diseases Study. There are many more RAABs than other eye health survey types, in part because the infrastructure and survey support ICEH provides makes them simpler and cheaper to complete than bespoke surveys. In the most recent 2020 VLEG estimates, RAAB data made up 46% and 61% of all data sources used to estimate global and regional blindness prevalence and causes respectively [14,15]. These outputs are used to track global trends, and populate the IAPB Vision Atlas, an interactive database that is a key resource for global eye health advocacy efforts.
Additionally, ICEH leads in generating global estimates for eCSC, and supports the WHO and VLEG in generating global estimates for eREC, both using mostly RAAB data [8]. The WHO have set a target of a 30% increase in eCSC for all countries by 2030, alongside a 40% increase in eREC [16]. In 2022, we published a secondary analysis of 148 RAAB surveys in 55 countries and contributed RAAB data to a similar paper by VLEG to set the baseline for both targets – 100% of eCSC data and 87% of eREC data came from RAAB [8,17]. We are currently working with WHO and VLEG to generate new estimates of eCSC and eREC for 2025 based on RAAB and non-RAAB data to provide new insight into progress towards the 2030 target.
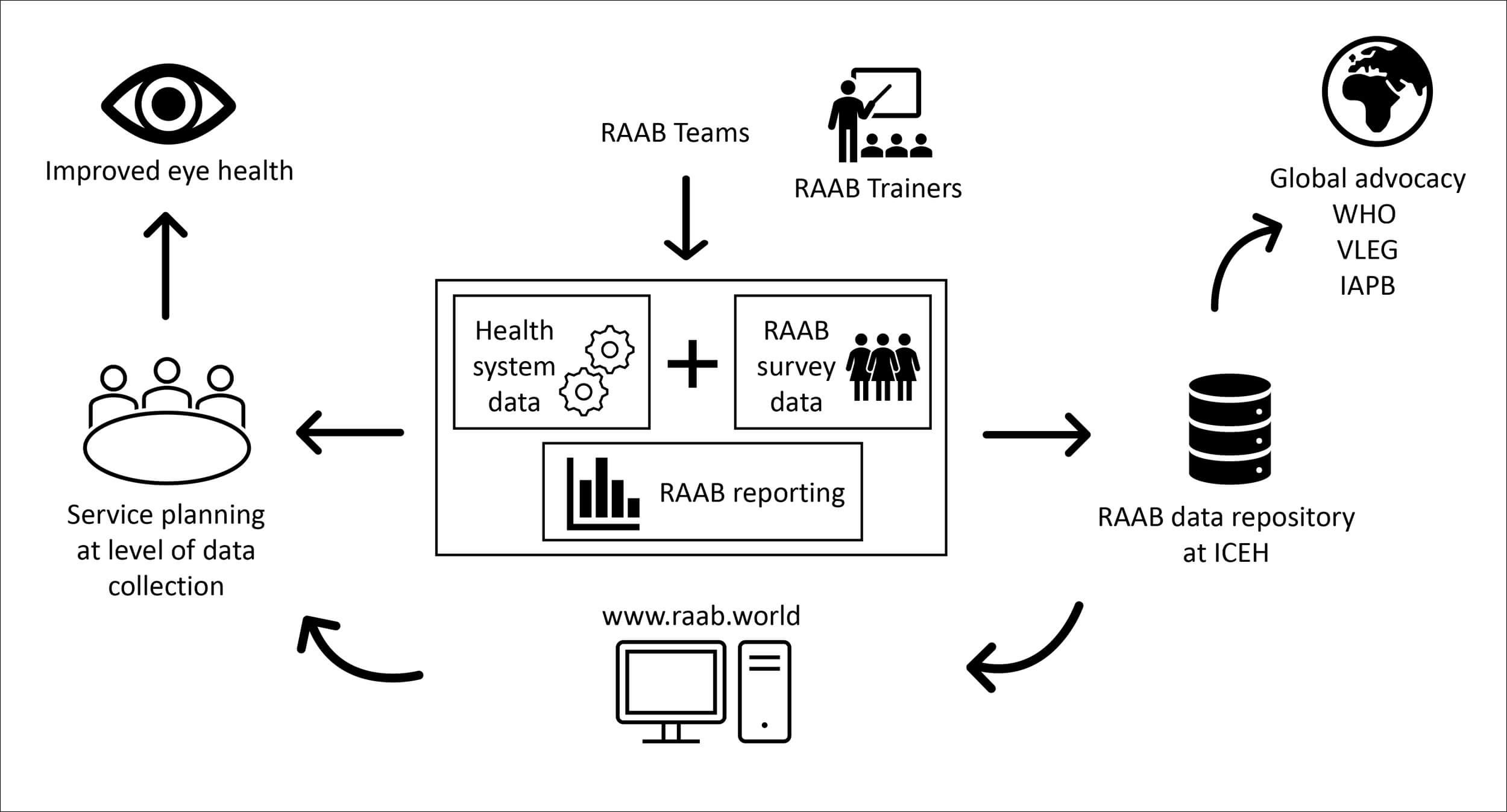
Figure 2: RAAB ecosystem.
A tool developed with the sector, for the sector
RAAB is a cornerstone of the global eye health data ecosystem, providing crucial data for local planning, and the majority of data points used to estimate prevalence and causes of vision impairment and blindness at the global level (Figure 2). As the global standard for population eye health reporting, RAAB needs to be responsive to emerging trends and needs. In 2025, we will continue development of our health systems and health economics modules, and conduct a stakeholder prioritisation study, to gather input on priority areas for research and development for the next five years. We anticipate interest in digital image capture and the use of artificial intelligence to identify pathology, and in strategies for sampling people under 50 for estimates of refractive error or non-vision-impairing conditions. Resourcing the ongoing research, development and maintenance of RAAB by ICEH is a challenge in the current climate but continues to be a priority given its central role in global eye health.
References
1. Limburg H, Kumar R, Indrayan A, Sundaram KR. Rapid assessment of prevalence of cataract blindness at district level. Int J Epidemiol 1997;26(5):1049–154.
2. Dineen B, Foster A, Faal H. A proposed rapid methodology to assess the prevalence and causes of blindness and visual impairment. Ophthalmic Epidemiol 2006;13(1):31–4.
3. Kuper H, Polack S, Limburg H. Rapid assessment of avoidable blindness. Community Eye Health 2006;19(60):68–9.
4. Oye J, Mactaggart I, Polack S, et al. Prevalence and Causes of Visual Impairment in Fundong District, North West Cameroon: Results of a Population-Based Survey. Ophthalmic Epidemiol 2017;24(6):394–400.
5. McCormick I, Kim MJ, Hydara A, et al. Socioeconomic position and eye health outcomes: identifying inequality in rapid population-based surveys. BMJ open 2023;13(3):e069325.
6. Ramke J, Zwi AB, Silva JC, et al. Evidence for national universal eye health plans. Bulletin of the World Health Organization 2018;96(10):695–704.
7. Burton MJ, Ramke J, Marques AP, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob Health 2021;9(4):e489–e551.
8. McCormick I, Butcher R, Evans JR, et al. Effective cataract surgical coverage in adults aged 50 years and older: estimates from population-based surveys in 55 countries. Lancet Glob Health 2022;10(12):e1744–e1753.
9. McCormick I, Mactaggart I, Bastawrous A, et al. Effective refractive error coverage: an eye health indicator to measure progress towards universal health coverage. Ophthalmic Physiol Opt 2020;40(1):1–5.
10. McCormick I, Butcher R, Ramke J, et al. The Rapid Assessment of Avoidable Blindness survey: Review of the methodology and protocol for the seventh version (RAAB7). Wellcome Open Res 2024;9:133.
11. Mactaggart I, Limburg H, Bastawrous A, et al. Rapid Assessment of Avoidable Blindness: looking back, looking forward. BJO 2019;103(11):1549–52.
12. Wilkinson MD, Dumontier M, Aalbersberg IjJ, et al. The FAIR Guiding Principles for scientific data management and stewardship. Sci Data 2016;3(1):160018.
13. https://www.R-project.org [Link last accessed September 2025]
14. Steinmetz JD, Bourne RRA, Briant PS, et al. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health 2021;9(2):e144–e160.
15. Bourne R, Steinmetz JD, Flaxman S, et al. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet Glob Health 2021;9(2):e130–e143.
16. Keel K, Müller A, Block S, et al. Keeping an eye on eyecare: monitoring progress towards effective coverage. The Lancet Glob Health 2021;9(10):e1460–e1464.
17. Bourne RRA, Cicinelli MV, Sedighi T, et al. Effective refractive error coverage in adults aged 50 years and older: estimates from population-based surveys in 61 countries. Lancet Glob Health 2022;10(12):e1754–e1763.













